The World Health Organization (WHO) defines Coronary Heart Disease (CHD), also known as Coronary Artery Disease (CAD), as a cardiovascular condition characterized by the narrowing or blockage of the coronary arteries. These arteries are responsible for supplying oxygen and nutrients to the heart muscle. CHD typically develops due to the accumulation of fatty deposits and plaque within the coronary arteries, a process known as atherosclerosis. The Epidemiology of CHD has been discussed in “The Global Burden of Coronary Heart Disease: A Comprehensive Overview“.
Pathophysiology
To begin understanding the pathophysiology of CHD, one must first comprehend how plaque forms.
The endothelium is typically followed by layers of tunica intima, tunica media, and tunica adventitia (composed of connective tissue) in the arteries that carry oxygenated blood to the heart, brain, and other organs.
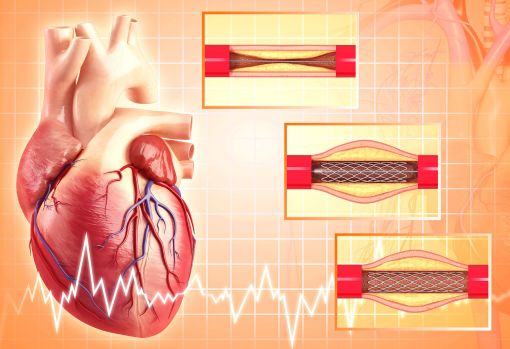
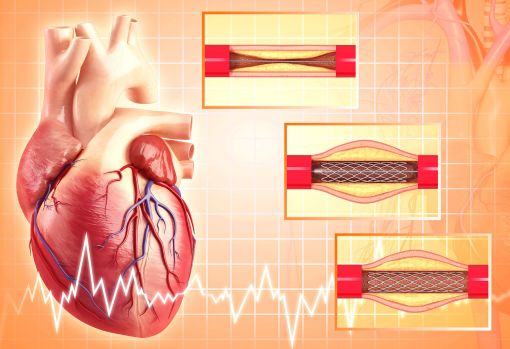
When there is a high level of circulating LDL in blood, it starts to enter the tunica intima layer of blood vessels, where it first becomes oxidized and then activates the receptors on the endothelial cells for leukocytes like monocytes These monocytes, via activated receptors, enter the tunica intima layer where they engulf they LDL molecules leading to the production of foam cells. These foam cells promote the proliferation and migration of smooth muscle cells from tunica media to tunica intima. Smooth muscle cells migrate and grow inside the intima while depositing more lipids. With fibroblasts, smooth muscle cells produce and secrete collagen, proteoglycans, elastin, and glycoproteins, forming a fibrous cap over cells and necrotic tissue known as plaque. The rupture of this plaque leads to thrombus formation, which causes the narrowing of arteries.
WHO ARE AT RISK?
Factors that increase the risk of CHD
- Cigarette smoking
- Raised serum cholesterol
- Hypertension
- Diabetes
- Abdominal obesity
- Increased personal stress
Factors that decrease the risk of CHD
- Regular consumption of fresh fruit and vegetables
- Regular exercise
- Moderate alcohol consumption
- Modification of factors that increase the risk of CHD
Clinical manifestation
- Chest pain or discomfort (angina)
- Weakness, light-headedness, nausea (feeling sick to your stomach), or a cold sweat.
- Pain or discomfort in the arms or shoulder.
- Shortness of breath.
- Vomiting
- Cough
DIAGNOSTIC TESTS
- Coronary angiography (gold standard)
- Myocardial scintigraphy (isotope scanning)
- Stress echocardiography (ultrasound)
- Electrocardiogram (ECG)
- Magnetic resonance imaging (MRI)
- Multi-slice CT scanning


TREATMENT AND MANAGEMENT
Following are the CHD Treatment Options or options for Managing Coronary Heart Disease:
ANTIPLATELET THERAPY
Thrombus development is one of the main issues caused by atheromatous plaque. This results in plaque growth and could lead to myocardial infarction. Anti-platelet drugs include:
- Aspirin (NSAID)
When taken chronically in doses of 75 mg daily, aspirin irreversibly inhibits platelet COX-1 and thromboxane synthesis. The optimum maintenance dose is between 75 and 150 mg per day, with lower doses offering very little protection against cardiac risk and larger ones raising the risk of gastrointestinal side effects.
- Clopidogrel.
Clopidogrel inhibits ADP activation of platelets and is useful as an alternative to aspirin in patients who are allergic or cannot tolerate aspirin. The average dose is 300 mg once, followed by 75 mg daily.
Anti -hypertensives
A large portion of pharmacological therapy is focused on reducing the heart’s workload and, to a lesser extent, boosting coronary blood flow; this relieves symptoms and enhances prognosis.
- ACE inhibitors(captopril)
In addition to the vasodilation caused by inhibiting the production of angiotensin II, ACE inhibitors have anti-inflammatory, antithrombotic and antiproliferative properties. For Capoten (captopril), a target maintenance dose of 50 mg t.i.d. is advised for long-term use in patients with myocardial infarction.
- β-Blockers
They reduce myocardial oxygen demand by blocking β-adrenergic receptors, decreasing the heart rate and force of left ventricular contraction and lowering blood pressure. Drugs include bisoprolol (Concor) 2.5mg BID or 5mg OD.
- Calcium channel blockers
Longer-acting dihydropyridines, like amlodipine and felodipine, or longer-acting formulations, like nifedipine LA, have shown symptom-relieving potential similar to -blockers. Short-acting dihydropyridine CCBs have been implicated in the exacerbation of angina due to the phenomenon of “coronary steal.”
Vasodilators
- Nitrates:
Organic nitrates are useful in treating angina because they increase blood flow in collateral coronary vessels, shift blood away from the epicardium to the endocardium, and widen veins and arteries to a lesser amount. E.g Angised 0.5 to 1 mg sublingually taken 5 to 10 minutes before a precipitating event
- Nicorandil
Nicorandil is a substance that has nitrate-like characteristics but also opens ATP-dependent potassium channels.