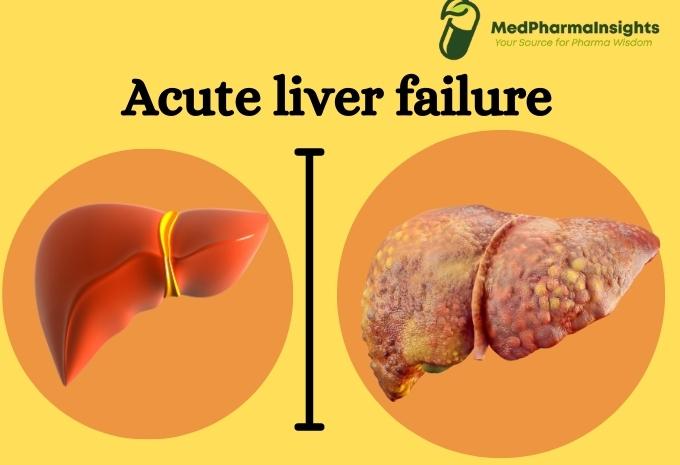
The liver is an incredibly resilient organ, but when it fails, it can have serious and potentially life-threatening consequences. Liver failure is a complex condition that can be broadly categorized into two main types: acute liver failure (ALF) and chronic liver failure (CLF). In this blog post, we will delve into the differences between these two forms of liver failure, their causes, symptoms, and potential treatments.
Acute liver failure
Acute liver failure is a rare disease. It takes place when your liver’s capacity to function starts to decline suddenly. Acute liver disease is a reversible event of hepatocyte injury that typically recovers on its own without leaving any clinical aftereffects.
This is an uncommon syndrome with a sudden decrease in liver function, coagulopathy (where there is a change in the blood’s capacity to coagulate i.e( form clots), and an accompanying encephalopathy (altered mentation). Acute liver failure (ALF) has a high mortality and morbidity rate and may call for an urgent liver transplant. Fulminant hepatic failure, sometimes referred to as acute liver failure.
What causes ALF ?
- Acetaminophen overdose
The most frequent cause of acute liver failure is taking too much acetaminophen (Tylenol, among other products). Acetaminophen is known as paracetamol outside of the US. After taking one extremely high dose of acetaminophen, acute liver failure can happen. The daily safe dosage of acetaminophen is 4g.
- Herbs
Acute liver failure has been associated with herbal medications and supplements such kava, ephedra, skullcap, and pennyroyal.
- Mushroom
The deadly wild mushroom Amanita phalloides, which is occasionally mistaken for one that is safe to consume, is one of the toxins that can result in abrupt liver failure.
- Autoimmune disease
Autoimmune hepatitis, a condition in which your immune system targets liver cells and injures and inflames them, can result in liver failure.
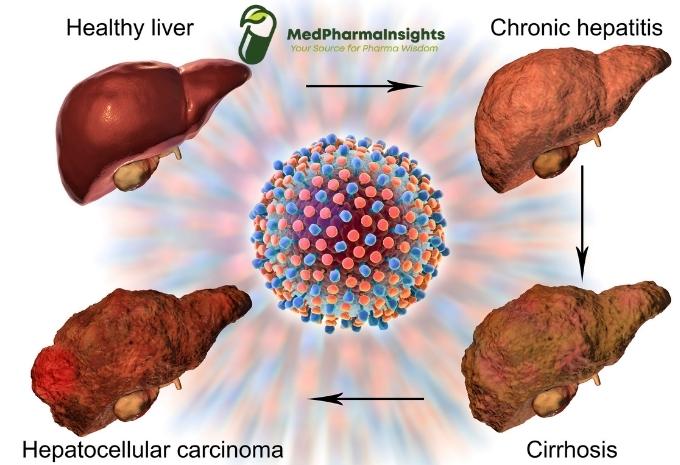
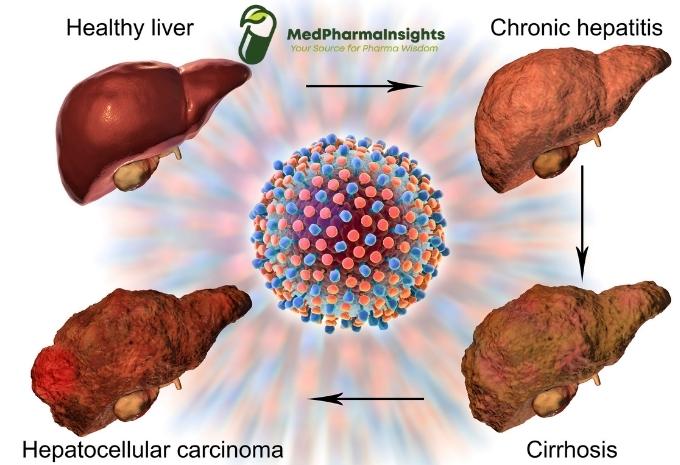
Chronic liver disease
Chronic liver disease arises when the liver experiences long-term structural changes due to cell injury, which destroys the normal architecture of the liver. Cirrhosis is a long-term (chronic) liver disease. This frequently develops into cirrhosis, when fibrous scars separate the liver cells into nodules of regenerating tissue. Once chronic liver disease worsens, patients run the risk of developing hepatocellular cancer, portal hypertension, or liver failure. Cirrhosis is a complication of chronic liver disease, regardless of the origin, and it can take anywhere between five and twenty years or longer to develop.
What causes CLF?
- Chronic Hepatitis B or C: These viral infections can lead to cirrhosis and CLF over an extended period if left untreated.
- Alcoholic Liver Disease: Excessive and prolonged alcohol consumption can result in alcoholic liver disease, which can progress to cirrhosis and CLF.
- Non-Alcoholic Fatty Liver Disease (NAFLD): Accumulation of fat in the liver can progress to non-alcoholic steatohepatitis (NASH), eventually leading to cirrhosis and CLF.
- Autoimmune Liver Diseases: Conditions like autoimmune hepatitis, primary biliary cholangitis (PBC), and primary sclerosing cholangitis (PSC) can lead to CLF if not properly managed.
Symptoms and Diagnosis
Both ALF and CLF share some common symptoms, such as jaundice (yellowing of the skin and eyes), fatigue, abdominal pain, and nausea. However, the timeline of symptom development and the underlying causes can differ significantly.
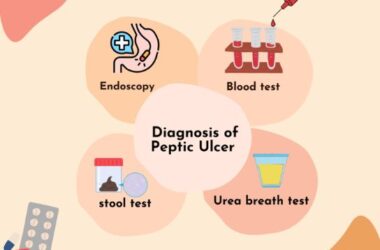
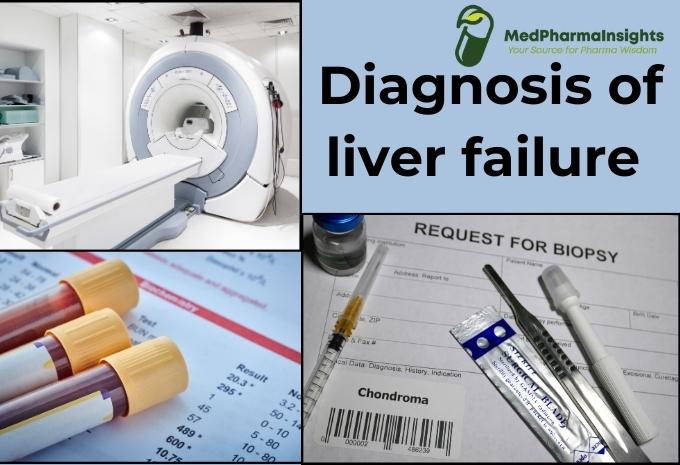
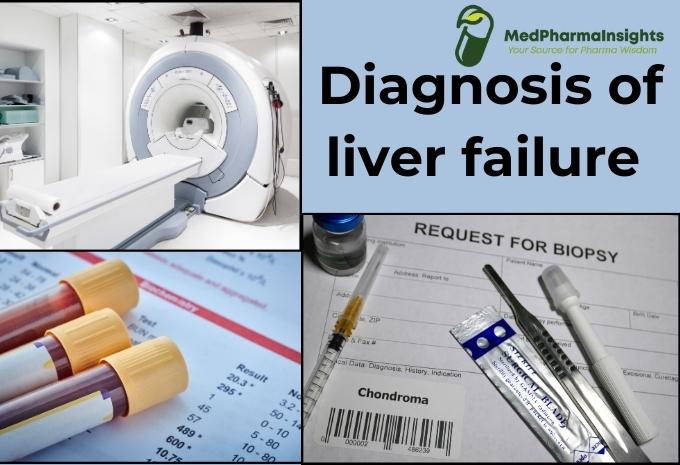
Diagnosis typically involves blood tests, imaging studies, and sometimes a liver biopsy to determine the type of liver failure and its severity.
Diagnosis
- Medical History and Physical Examination: The diagnostic process typically begins with a thorough medical history to identify potential causes and risk factors. A physical examination may reveal signs such as jaundice (yellowing of the skin and eyes), abdominal tenderness, and changes in mental status.
- Blood Tests: Blood tests are essential for assessing liver function and identifying abnormalities. Specific tests include:
- Liver function tests: These measure liver enzymes, bilirubin, and other markers of liver health.
- Coagulation studies: To assess blood clotting function, as impaired clotting is common in ALF.
- Serology: Testing for viral hepatitis (e.g., Hepatitis A, B, C), autoimmune markers, and other potential causes.
- Imaging: Imaging studies such as ultrasound, computed tomography (CT) scans, or magnetic resonance imaging (MRI) may be performed to visualize the liver and surrounding structures, helping to identify any structural abnormalities or complications.
- Liver Biopsy: In some cases, a liver biopsy may be necessary to assess the extent of liver damage and help determine the underlying cause of ALF. However, this is less common due to the critical condition of ALF patients.
Diagnosis of Chronic Liver Failure (CLF):
- Medical History and Physical Examination: As with ALF, a comprehensive medical history and physical examination are the initial steps in diagnosing CLF. The healthcare provider will inquire about risk factors and symptoms.
- Blood Tests: Blood tests are crucial for assessing liver function, identifying underlying causes, and monitoring disease progression. Common blood tests include:
- Liver function tests: These measure enzymes, bilirubin, and other liver markers.
- Viral hepatitis serology: To check for the presence of hepatitis B and C viruses.
- Autoimmune markers: To detect autoimmune liver diseases.
- Fibrosis markers: Blood tests like FibroScan or ELF (Enhanced Liver Fibrosis) can assess the degree of liver fibrosis or scarring.
- Imaging: Imaging studies such as ultrasound, CT scans, or MRI may be used to visualize the liver’s structure and identify complications like cirrhosis, portal hypertension, or liver tumors.
- Liver Biopsy: A liver biopsy may be performed in certain cases to confirm the diagnosis, assess the extent of liver damage, and guide treatment decisions. However, non-invasive methods, like fibrosis scoring, are increasingly used to evaluate liver fibrosis.
- Endoscopy: Upper gastrointestinal endoscopy may be recommended to assess for varices (enlarged veins) in the esophagus or stomach, a common complication of advanced liver disease.
- CT or MRI Liver Elastography: These imaging techniques can provide non-invasive assessments of liver stiffness, which can indicate the degree of fibrosis or cirrhosis.
- Liver Function Tests Over Time: Serial liver function tests and monitoring of key markers over time help assess disease progression and the effectiveness of treatment.
Treatment & Management of liver failure
Treatment Approaches for Acute Liver Failure (ALF):
- Hospitalization: Acute liver failure is a medical emergency, and individuals diagnosed with ALF should be hospitalized immediately for close monitoring and treatment.
- Supportive Care: The primary goal of treatment for ALF is to provide supportive care to stabilize the patient and prevent further liver damage. This includes monitoring vital signs, providing oxygen therapy, and addressing any complications such as bleeding or infections.
- Identifying and Treating the Underlying Cause: Identifying the underlying cause of ALF is crucial. For example, if ALF is caused by a drug overdose, the administration of antidotes or medications like N-acetylcysteine may be necessary to counteract the toxic effects.
- Liver Transplantation: In severe cases of ALF where the liver is irreversibly damaged and the patient’s condition deteriorates rapidly, a liver transplant may be the only lifesaving option. Liver transplantation involves replacing the damaged liver with a healthy one from a donor.
- Supportive Medications: Medications may be prescribed to manage symptoms and complications. For instance, intravenous fluids can help maintain hydration, and lactulose may be used to treat hepatic encephalopathy (a neurological complication of liver failure).
Treatment Approaches for Chronic Liver Failure (CLF):
- Managing the Underlying Cause: Treating the underlying cause of chronic liver failure is essential. For example, antiviral medications may be prescribed to manage chronic hepatitis B or C infections. Lifestyle modifications, such as avoiding alcohol and adopting a healthy diet, are often recommended for conditions like alcoholic liver disease and non-alcoholic fatty liver disease (NAFLD).
- Dietary Changes: A diet low in salt and easy on the liver is typically advised for individuals with CLF. Reducing dietary protein may be necessary in cases of hepatic encephalopathy. In some cases, nutritional supplements may be recommended to address malnutrition.
- Medications: Medications may be prescribed to manage symptoms and complications associated with CLF. For example, diuretics can help reduce fluid buildup (ascites) in the abdomen, and beta-blockers may be used to lower blood pressure in cases of portal hypertension.
- Liver Transplantation: In advanced stages of chronic liver failure, when the liver is severely damaged and the patient’s health continues to deteriorate despite medical management, liver transplantation may be the best option. Transplantation offers the chance of a new, healthy liver and improved survival.
- Regular Monitoring: Individuals with CLF require ongoing monitoring by healthcare providers to assess liver function, manage complications, and adjust treatments as needed.
- Preventing Complications: Preventing and managing complications is crucial in CLF. Vaccinations for conditions like Hepatitis A and B are often recommended to prevent further liver damage. Additionally, medications and lifestyle changes may be prescribed to manage conditions like portal hypertension and hepatic encephalopathy.