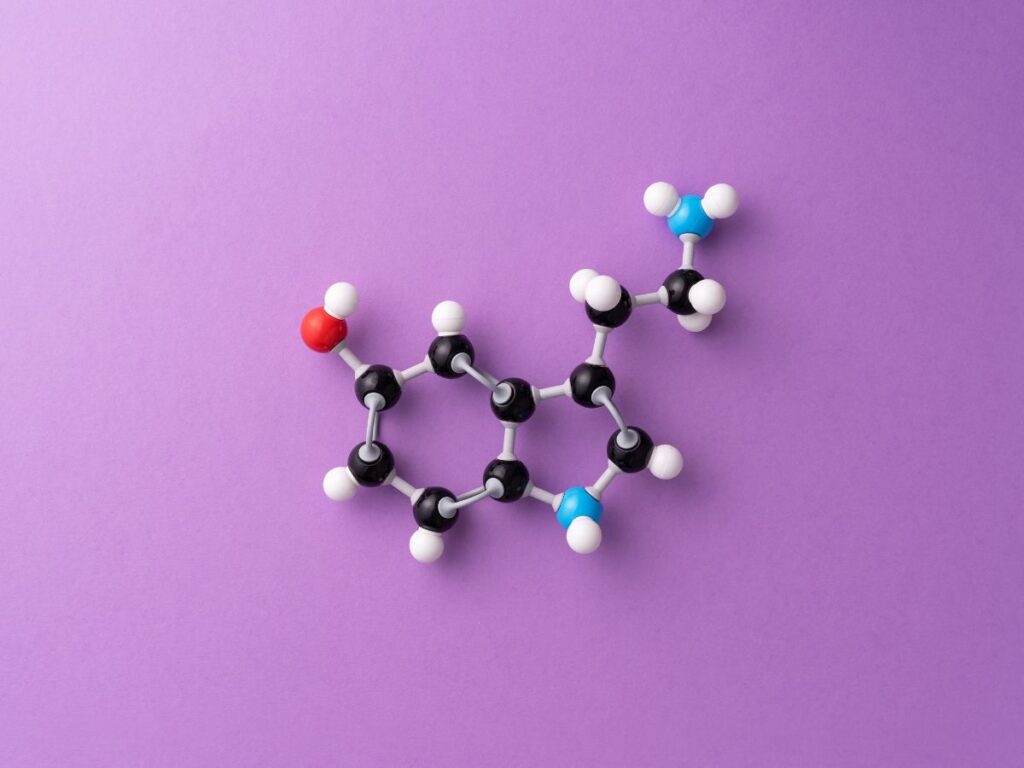
PD stands for Parkinson’s disease. Parkinson’s disease is a progressive and neurodegenerative disorder that primarily affects motor function but can also lead to a wide range of non-motor symptoms. It is characterized by the gradual degeneration of dopamine-producing neurons in a region of the brain called the substantia nigra. Dopamine is a neurotransmitter that plays a critical role in motor control and coordination.
Epidemiology
Over 65 years of age, 1% of people have Parkinson’s disease; this number rises to 2% over 80 years of age. However, one in twenty patients are diagnosed prior to their forty. Parkinson’s disease affects an estimated 110,000 persons in the United Kingdom. A slight male-to-female predominance has been reported by the majority of epidemiological investigations.A prevalent kind of symptomatic Parkinsonism is drug-induced Parkinsonism. Ten to fifteen percent of people who are exposed to drugs that block dopamine receptors, such as certain labyrinthine sedatives and neuroleptics, experience it. Compared to Western nations, the prevalence of Parkinson’s disease (PD) was marginally lower in Asian nations.
Etiology
- Genetics: individuals with a family history of Parkinson’s disease and genetic mutations, such as those in the LRRK2 and GBA genes, In recent years, eight genetic loci and a further four genes (parkin, DJ-1, PINK1 and LRRK-2) have been identified have been linked to an increased risk of Parkinson’s. Mutation in the gene coding for a synaptic protein called α-synuclein is a major component of the pathological hallmark of Parkinson’s disease
- Age: Parkinson’s disease is more common in older adults. The risk increases with age, and most cases are diagnosed after the age of 60.
- Environmental Factors: In the 1980s, environmental variables gained prominence when drug addicts trying to make pethidine unintentionally created a poison known as MPTP (1-methyl-4-phenyl1,2,3,6-tetrahydropyridine). MPTP ingestion or inhalation quickly resulted in a severe Parkinsonian state that was identical to the latter stages of Parkinson’s disease.
- Inflammation: Inflammation in the brain may contribute to the progression of Parkinson’s disease.
- Head Trauma: There is some evidence that a history of head injuries, especially repeated head trauma, may increase the risk of developing Parkinson’s disease.
- Viral Infections: Some studies have suggested a possible link between viral infections and the development of Parkinson’s disease, but this connection is still being investigated.
Pathophysiology
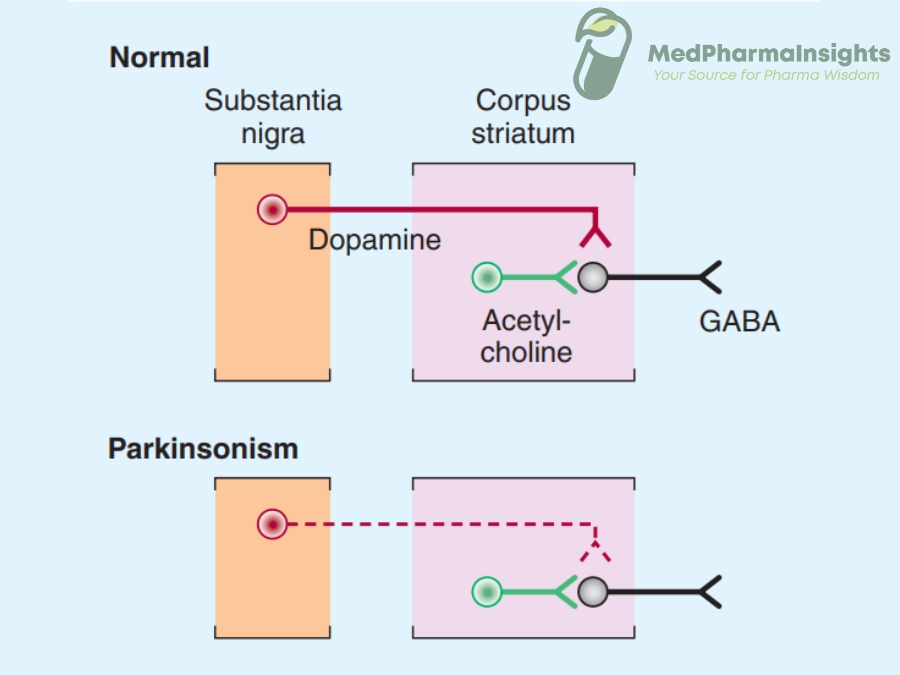
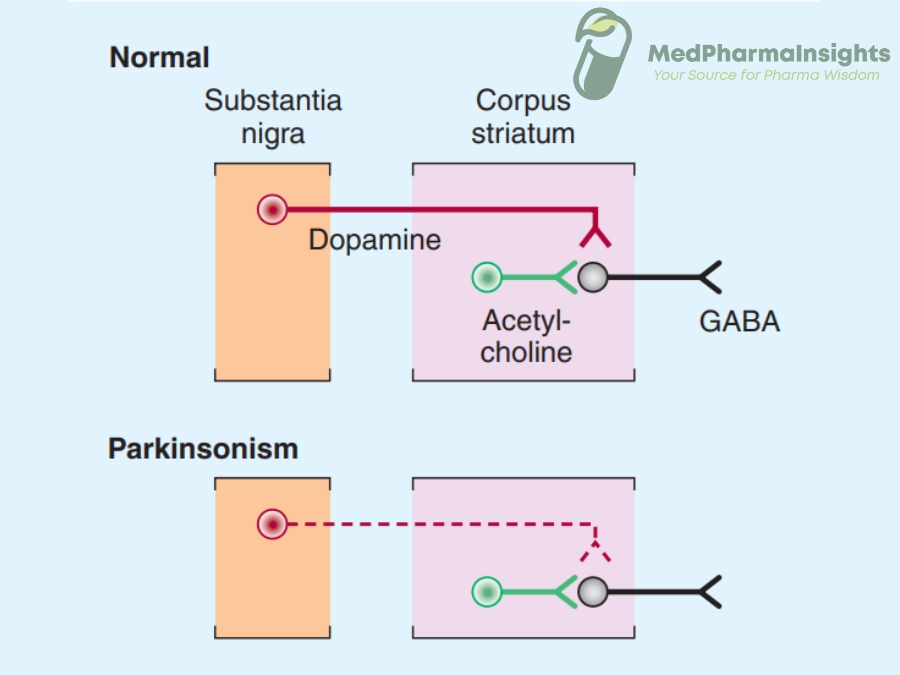
Basal ganglia : The basal ganglia is a group of interconnected nuclei (clusters of neurons) located deep within the brain. It helps to regulate and modulate voluntary motor movements, including the initiation, inhibition, and coordination of these movements. The main components of the basal ganglia include: Striatum (Caudate Nucleus and putamen nucleus ), Globus Pallidus, Subthalamic Nucleus (STN) and Substantia Nigra.
The key feature of PD is the progressive degeneration of dopamine-producing neurons in the substantia nigra, a region deep within the brain. Substantia nigra is a part of basal ganglia , a cluster of nuclei responsible for motor control. As the neurons in substantia nigra degenerate, there is a significant reduction in the production of dopamine, a neurotransmitter crucial for coordinating smooth and controlled movements.
This dopamine depletion disrupts the delicate balance of neurotransmission within the basal ganglia. In the absence of sufficient dopamine, the inhibitory signals that regulate movement are impaired, leading to overactivity in certain neural pathways and underactivity in others.
This disruption manifests as the hallmark motor symptoms of PD, including resting tremors, bradykinesia (slowness of movement), rigidity, and postural instability. Additionally, the formation of abnormal protein aggregates known as Lewy bodies within neurons further contributes to cell dysfunction and neuronal damage.
Clinical features
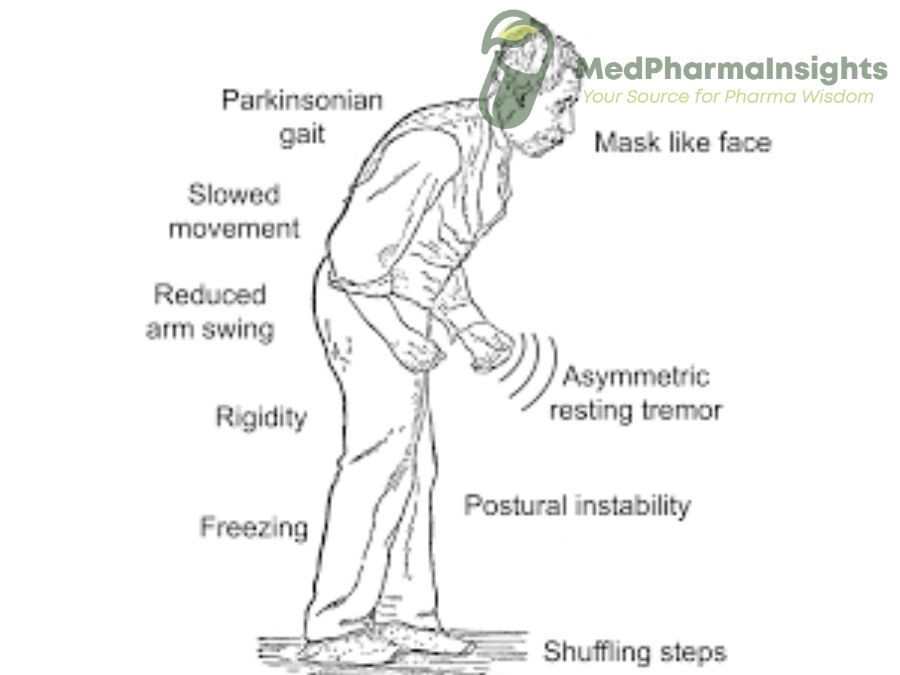
A- Motor
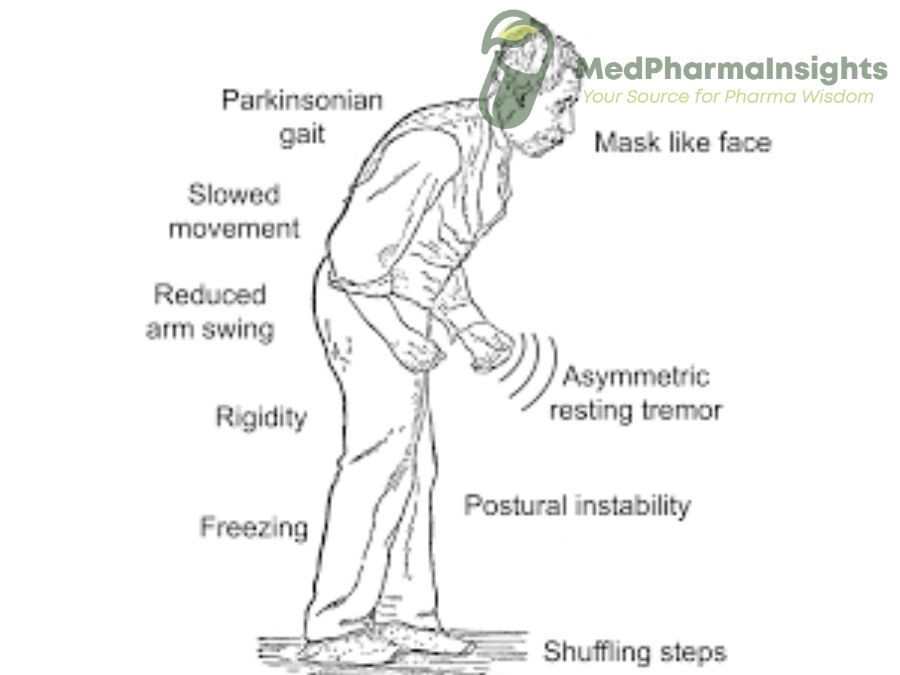
1- Bradykinesia
This refers to slowness of movement. People with Parkinson’s may have difficulty initiating and executing voluntary movements. Simple tasks can become time-consuming.
2- Rest tremor
Resting tremors, typically in one hand or foot, are a hallmark symptom of Parkinson’s. These tremors often have a “pill-rolling” quality, where the thumb and fingers move in a circular motion. The rest tremor is a rhythmic movement with a frequency of 4–6 Hz (cycles/s), typically noticed with the patient at rest.
3- Extrapyramidal rigidity (so-called lead pipe and/or cog-wheel):
Muscle stiffness or rigidity can make movement and joint flexibility challenging.
4- Postural instability:
One of the latter symptoms of Parkinson’s disease is postural instability, which is characterized by a loss of reflexive balance and a propensity to fall. When walking, there can be a flexed truncal posture and a decrease of arm swing. Reduced facial expression and blink frequency, along with somewhat hypophonic (low loudness) speech and monotonous speech, might cause serious communication problems. Writing gets tiny and hardly readable (micrographia).
B- Non-motor features
- Autonomic dysfunction
- Urogenital difficulties
- postural hypotension
- Depression
- Dementia
- Loss of Sense of Smell: Hyposmia (reduced sense of smell) or anosmia (loss of the sense of smell) is common in Parkinson’s.
Diagnosis
Copper studies: In the context of medicine and healthcare, typically refer to a set of diagnostic tests and investigations aimed at measuring the levels of copper in the body or assessing its role in specific health conditions.
- FP-CIT SPECT: When there is difficulty in distinguishing Parkinson’s disease from essential tremor, a form of functional imaging called FP-CIT SPECT (also known as DaTSCAN) may be useful, as this technique can sensitively identify loss of nigrostriatal dopaminergic terminals in the striatum
- Brain imaging: It might be essential to perform brain imaging using magnetic resonance imaging (MRI) or computed tomography (CT) to rule out hydrocephalus, cerebrovascular illness, or abnormalities in the basal ganglia that could indicate a metabolic etiology.
- copper studies
- DNA testing
Management of PD
Parkinson’s Disease (PD) is a complex neurological disorder that primarily affects movement, and while it is currently incurable, there are several treatment approaches aimed at managing its symptoms and improving the quality of life for individuals living with the condition. Treatment of PD is highly individualized and may involve a combination of the following strategies:
1. Medication:
- Levodopa: Levodopa, often combined with carbidopa (Sinemet), is the most effective medication for managing motor symptoms of PD. It is a precursor to dopamine and helps replenish dopamine levels in the brain, reducing bradykinesia, rigidity, and tremors.
- Dopamine Agonists: These medications mimic the effects of dopamine in the brain and may be used as initial therapy or in combination with levodopa.
- MAO-B Inhibitors: Monoamine oxidase type B (MAO-B) inhibitors, such as rasagiline and selegiline, can help increase dopamine levels by inhibiting its breakdown.
- Anticholinergics: These medications can help control tremors by altering the balance of neurotransmitters in the brain.
2. Deep Brain Stimulation (DBS):
DBS is a surgical procedure in which electrodes are implanted into specific areas of the brain. These electrodes deliver electrical impulses to modulate abnormal brain activity and can effectively reduce motor symptoms in some individuals.
3. Physical and Occupational Therapy:
Physical therapy can help individuals with PD maintain and improve their mobility, balance, and strength.
4. Speech and Swallowing Therapy:
PD can affect speech and swallowing function. Speech therapy can help individuals maintain clearer communication, and swallowing therapy can prevent aspiration and improve overall safety during meals.