Hepatic encephalopathy is a neurological condition that happens when the liver is damaged and cannot remove toxins from the blood properly. This can lead to a buildup of toxins, especially ammonia, in the body, which affects the brain and causes problems like confusion, trouble speaking, and even coma in severe cases.
Pathophysiology behind Hepatic encephalopathy
When your liver is infected or damaged, it struggles to filter out dangerous substances from your blood. Ammonia, a waste product created when your body breaks down proteins, is one of these compounds.
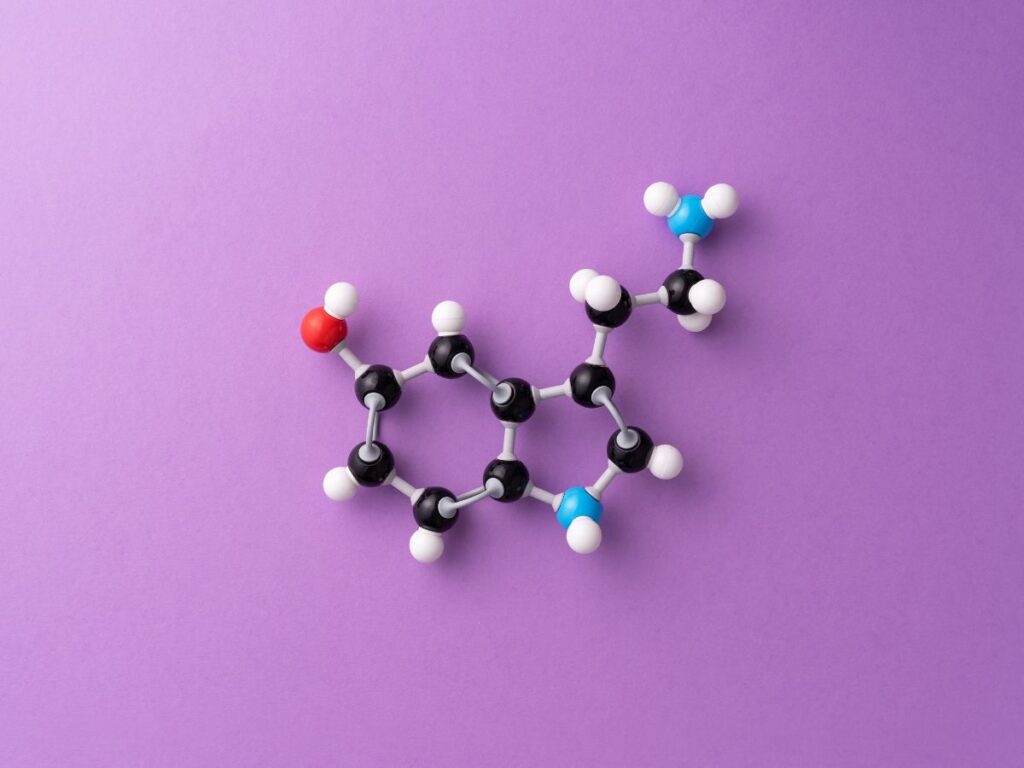
Your liver normally breaks down and eliminates ammonia safely. However, ammonia levels in your blood can increase if your liver is not working correctly. For the brain, ammonia is poisonous. It has an impact on how brain cells interact and communicate. For normal operation, the brain depends on a complex interplay of chemicals known as neurotransmitters.Ammonia disrupts this equilibrium. Neurotransmitters like glutamate and GABA are affected by it. These substances influence how your body functions and how your brain interprets information.
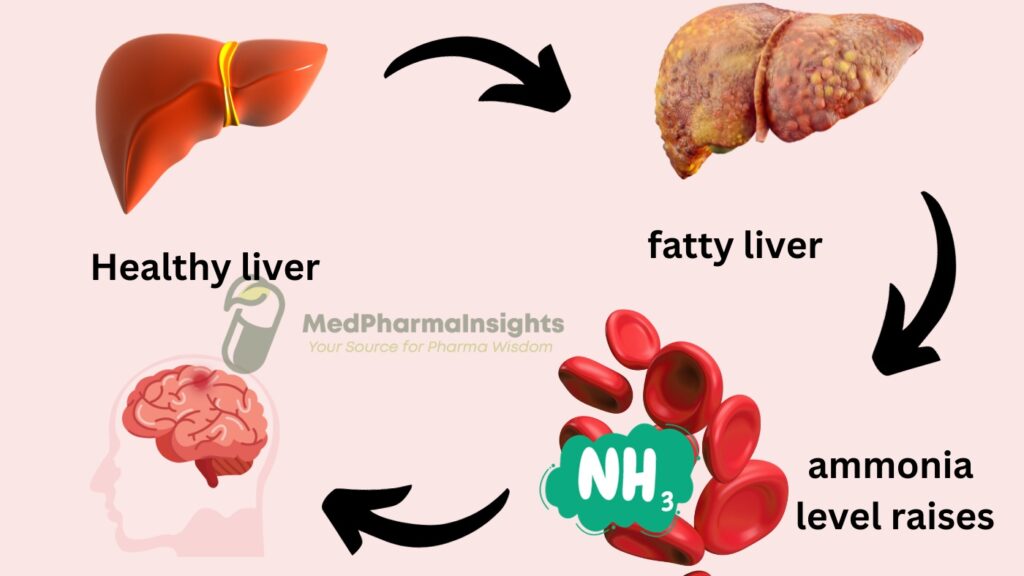
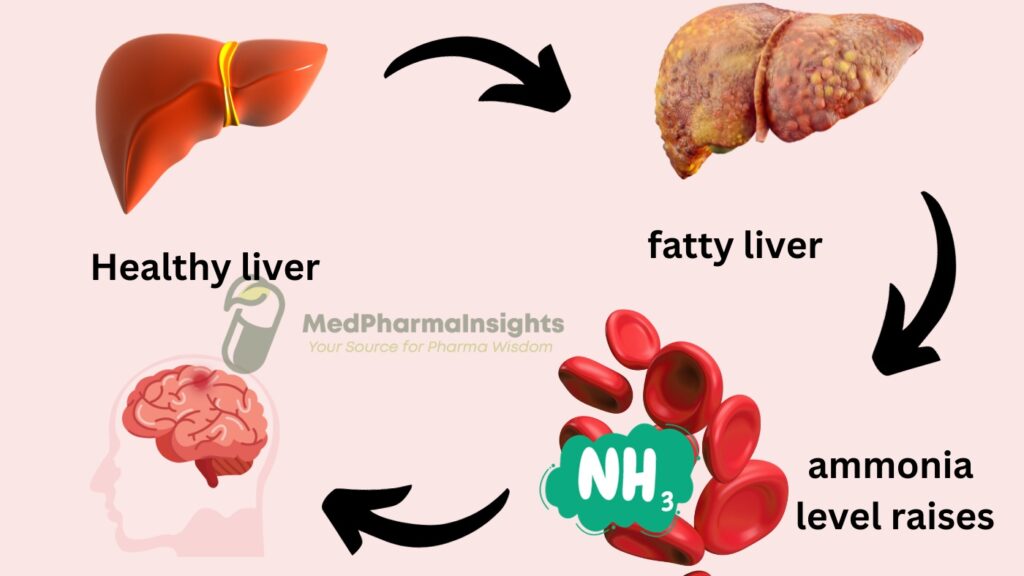
Numerous symptoms, including disorientation, difficulties thinking, shivering, and behavioral abnormalities, might be brought on by elevated ammonia levels and disrupted neurotransmitter balance. It may cause a coma in extreme circumstances. Blood-brain barrier weakness is another potential effect of hepatic encephalopathy, which acts as a protective shield surrounding your brain. This makes it possible for more poisons to enter the brain and exacerbate the symptoms.
Can your brain recover from hepatic encephalopathy?
Yes, Hepatic encephalopathy and its symptoms can be reversible with proper treatment.
Causes of hepatic encephalopathy
- Gastro-intestinal bleeding
- Infection (spontaneous bacterial peritonitis, other sites of sepsis)
- Hypokalaemia, metabolic alkalosis
- High protein diet
- Constipation
- Drugs, opioids and benzodiazepines
- Deterioration of liver function
- Post-surgical TIPS
Treatment and management
- Lactulose 15–30 mL orally 2–4 times daily Aim for 2–3 soft stools daily
- Metronidazole 400–800 mg orally daily in divided doses Metabolism impaired in liver disease
- Neomycin (Used less frequently now) 2–4 g orally daily in divided doses Maximum duration of 48 h
- Rifaxamin 550 mg twice daily Benefit demonstrated over 6 months use