Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder that affects millions of people worldwide. It can significantly impact an individual’s quality of life. In this comprehensive medical blog, we will explore IBS in detail, including its symptoms, causes, diagnosis, and management options.
Pathophysiology
The pathophysiology of Irritable Bowel Syndrome (IBS) is a complex and multifaceted process that involves various factors, including gastrointestinal motility, visceral hypersensitivity, the gut-brain axis, and immune system interactions. While the exact cause of IBS remains unclear, researchers have made significant strides in understanding the underlying mechanisms. Here’s an overview of the pathophysiology of IBS:
1- Altered Gut Motility:
IBS often involves abnormal contractions and motility of the muscles in the gastrointestinal (GI) tract. These abnormalities can lead to changes in bowel habits, including diarrhea, constipation, or alternating between the two. Factors such as increased sensitivity to certain foods or stress can trigger these abnormal motility patterns.
2- Visceral Hypersensitivity:
Many individuals with IBS have heightened sensitivity to sensations in their gut, a phenomenon known as visceral hypersensitivity. This means they may perceive normal gut contractions and sensations as pain or discomfort. Visceral hypersensitivity contributes to the abdominal pain and discomfort characteristic of IBS.
3- Gut-Brain Axis:
The gut and the brain communicate through a bidirectional pathway called the gut-brain axis. This communication plays a pivotal role in IBS. Stress, emotions, and psychological factors can influence gut function. For many individuals with IBS, stress and anxiety can trigger or exacerbate symptoms.
4- Immune System and Gut Microbiota:
Emerging research suggests that alterations in the gut microbiota and immune system interactions may play a role in IBS. An imbalance in the gut microbiome (dysbiosis) and immune system activation in response to gut microbes may contribute to gut inflammation and IBS symptoms in some individuals.
5- Low-Grade Inflammation (Possible):
While IBS is primarily considered a functional disorder, some studies have suggested the presence of low-grade inflammation in a subset of IBS patients. This inflammation may be related to immune system activation or alterations in the gut lining.
6- Genetic and Environmental Factors:
Genetic predisposition may play a role in susceptibility to IBS. Certain genetic variations are associated with an increased risk. Environmental factors, such as early life stress or exposure to gastrointestinal infections, can also contribute to the development of IBS in some cases.
7- Altered Brain-Gut Interactions:
Brain-gut interactions are disrupted in individuals with IBS. Abnormalities in the central nervous system’s processing of pain signals from the gut can lead to heightened perception of pain and discomfort.
It’s important to note that IBS is a heterogeneous condition, and not all individuals with IBS will have the same underlying pathophysiological mechanisms. Subtypes of IBS, such as diarrhea-predominant IBS (IBS-D), constipation-predominant IBS (IBS-C), or mixed-type IBS (IBS-M), may exhibit different patterns of pathophysiology.
Causes of IBS
The exact cause of IBS is not fully understood, but several factors are believed to contribute:
- Altered Gut Motility: Abnormal muscle contractions in the intestines can lead to diarrhea or constipation.
- Visceral Hypersensitivity: Some people with IBS may have heightened sensitivity to pain and discomfort in the intestines.
- Changes in Gut Microbiota: Alterations in the composition of gut bacteria may play a role in IBS.
- Dietary Triggers: Certain foods and beverages, such as high-fat foods, caffeine, alcohol, and artificial sweeteners, can exacerbate symptoms.
- Stress and Psychological Factors: Emotional stress and anxiety can worsen IBS symptoms in some individuals.
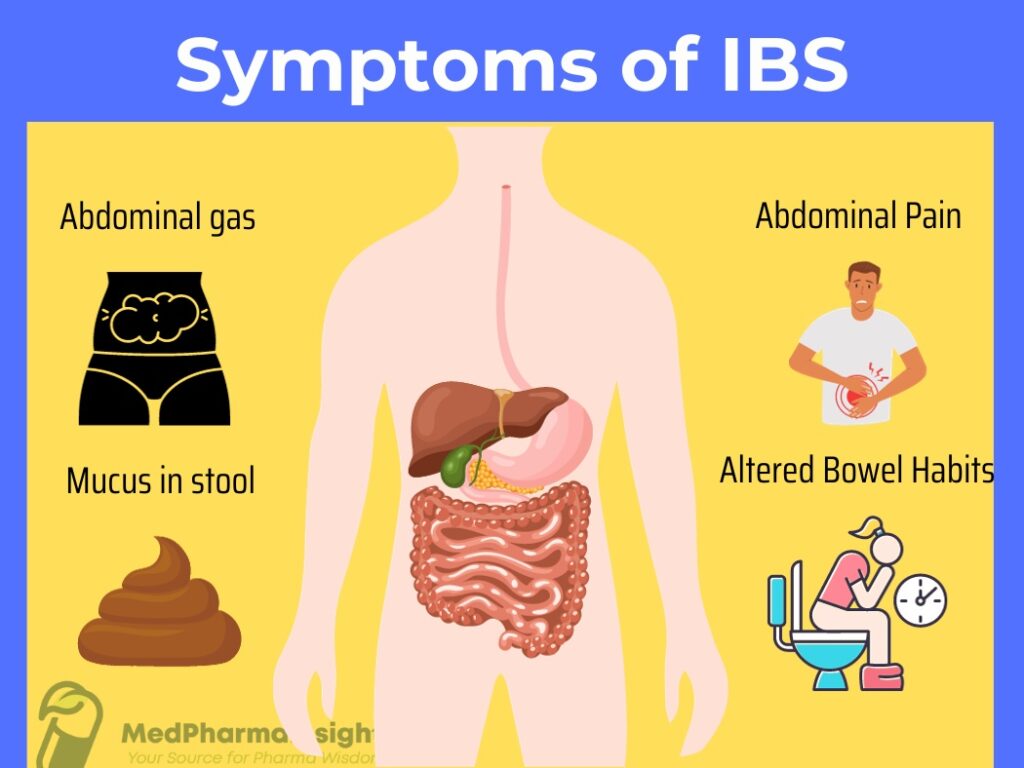
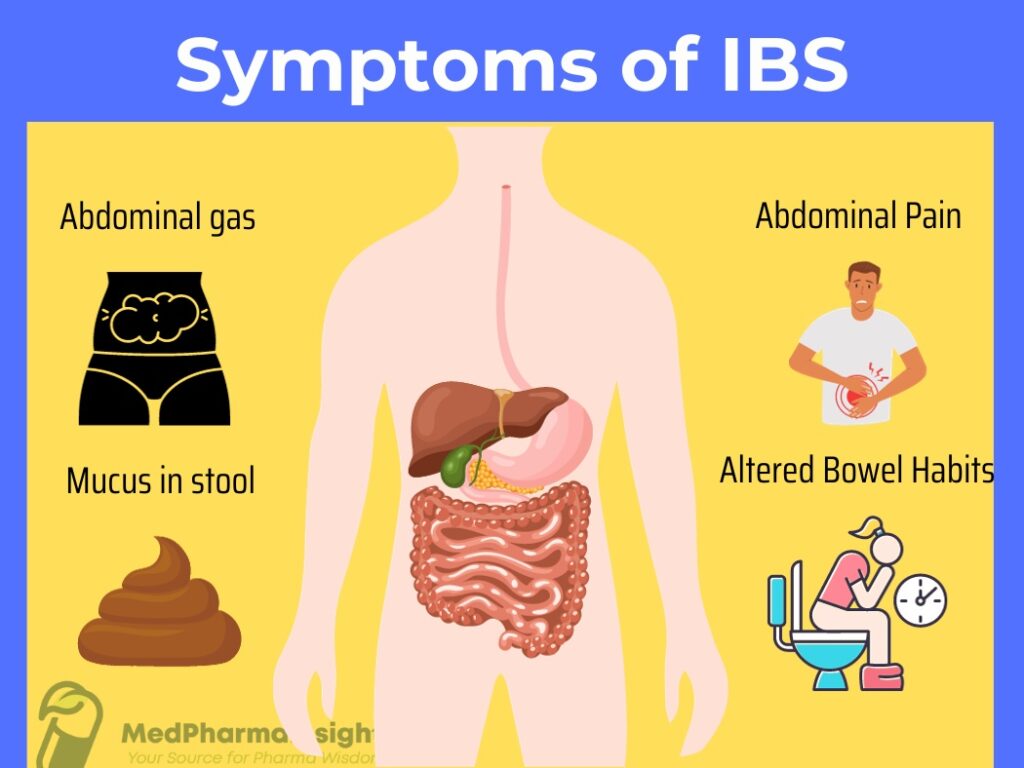
Symptoms of IBS
The hallmark of IBS is abdominal discomfort or pain associated with changes in bowel habits. Common symptoms include:
- bdominal Pain or Discomfort: Typically relieved after a bowel movement.
- Altered Bowel Habits: This can manifest as diarrhea, constipation, or a combination of both (mixed-type IBS).
- Bloating and Gas: Often accompanied by visible abdominal distention.
- Urgency: A sudden and compelling need to have a bowel movement.
- Mucus in Stool: Some individuals may notice increased mucus in their stool.
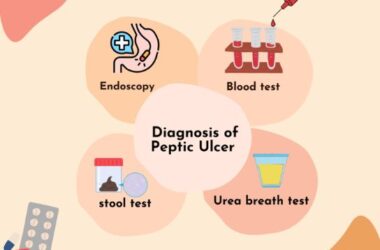
Diagnosis of IBS
Diagnosing IBS involves ruling out other potential gastrointestinal conditions through a combination of:
- Medical History: Your healthcare provider will ask about your symptoms, their duration, and any triggering factors.
- Physical Examination: This can help rule out other medical conditions.
- Diagnostic Tests: Blood tests, stool tests, and imaging studies may be performed to rule out other conditions like inflammatory bowel disease (IBD) or celiac disease.
- Colonoscopy or Endoscopy: In some cases, these procedures may be recommended to visualize the gastrointestinal tract and obtain biopsies.
Management of IBS
There is no one-size-fits-all approach to managing IBS, as treatment is tailored to individual symptoms and needs. Some strategies include:
- Dietary Changes: Identifying and avoiding trigger foods, following a low-FODMAP diet, or increasing fiber intake can help manage symptoms.
- Medications: Depending on your symptoms, your healthcare provider may recommend antispasmodic medications, laxatives, or medications to control diarrhea.
- Stress Management: Techniques such as relaxation exercises, counseling, or cognitive-behavioral therapy (CBT) can help manage stress-related symptoms.
- Probiotics: Some individuals find relief from IBS symptoms with certain probiotic supplements.
- Lifestyle Modifications: Regular exercise, adequate sleep, and a consistent meal schedule can help regulate bowel function.
- Psychotherapy: For individuals with significant psychological distress, therapy may be beneficial.
Conclusion
Irritable Bowel Syndrome is a common gastrointestinal disorder that can have a significant impact on a person’s daily life. Understanding its symptoms, causes, and management options is essential for individuals living with IBS and healthcare providers striving to provide effective care. While IBS is a chronic condition, many individuals can successfully manage their symptoms and improve their quality of life through various treatment strategies. If you suspect you have IBS or are experiencing persistent digestive symptoms, consult with a healthcare provider for a proper evaluation and personalized management plan.