Seizures may make life a difficult journey full of uncertainty and worry. However, there is hope in the form of efficient seizure management and treatment despite the unpredictability. It is crucial for people dealing with epilepsy or other seizure disorders to comprehend and navigate every aspect of their condition in order to find relief. In order to clarify the complex interactions between seizure management and treatment, we set out on a voyage of discovery in this blog. Our mission is to provide knowledge and assistance to empower people with seizures and their loved ones, from identifying the subtleties of seizure triggers to investigating cutting-edge remedies. Together, let’s set out on a journey of empathy, resiliency, and a common resolve to conquer in order to improve seizure management and treatment.
Convulsive seizures may appear frightening, although the person experiencing them is usually not in pain, does not remember what happened later, and is not gravely hurt. Rarely does one need emergency care. However, people should be made as comfortable as possible, ideally in a laying position (with their head cushioned and any tight clothes or neckwear loosened), or sitting with their backs to the floor. People should not be relocated during a seizure unless they are in a dangerous area, such as on a road, near a fire or hot heater, at the top of stairs, or by the edge of a body of water. It is advised to administer 10–20 mg of diazepam intravenously or rectal for adults, with smaller doses for children, if a seizure lasts more than 10 minutes, if there are multiple seizures, or if the seizure is exceptionally severe.
1- Status epilepticus : Seizure Management and Treatment
The first course of treatment of the seizures of status epilepticus is supportive and may involve the following:
-
- Keeping the patient’s blood pressure stable;
-
- Positioning them to prevent harm;
-
- Assisting with breathing;
-
- Correcting hypoglycemia.
Treatment of seizures:
Intravenous lorazepam or diazepam are among the drugs utilized.
When first-line medications have not produced the desired results, other medications such as midazolam may be prescribed. As an alternative, buccal midazolam has gained popularity and is being used more frequently, despite not having a license in the UK. Phenytoin, clonazepam, or phenobarbital sodium may be needed in extreme situations.
2- Febrile convulsions
Young people may experience febrile convulsions, which are convulsions linked to fever. The main goal of conservative management for brief febrile convulsions is to lower the child’s fever. Using tepid sponges and paracetamol is customary. To prevent brain injury, aggressive therapy is necessary for prolonged febrile convulsions that last 10 to 15 minutes or longer, or in a kid who has risk factors. Diazepam administered intravenously or as a rectal solution is the preferred medication. In certain children, such as those who have a history of extended seizures in the past or pre-existing risk factors, prophylactic care of febrile convulsions may be necessary.
As a child is experiencing a febrile seizure, remain composed and take the following actions:
-
- Lay that child down on a supple, level surface, facing sideways.
-
- Take off any tight apparel.
-
- Anything sharp or hard should be removed from the area.
-
- Begin keeping track of the seizure.
-
- Nothing should be placed in a child’s mouth.
-
- Keep the child unrestrained.
-
- Make a 911 call if the seizure lasts more than five minutes.
Long-term treatment
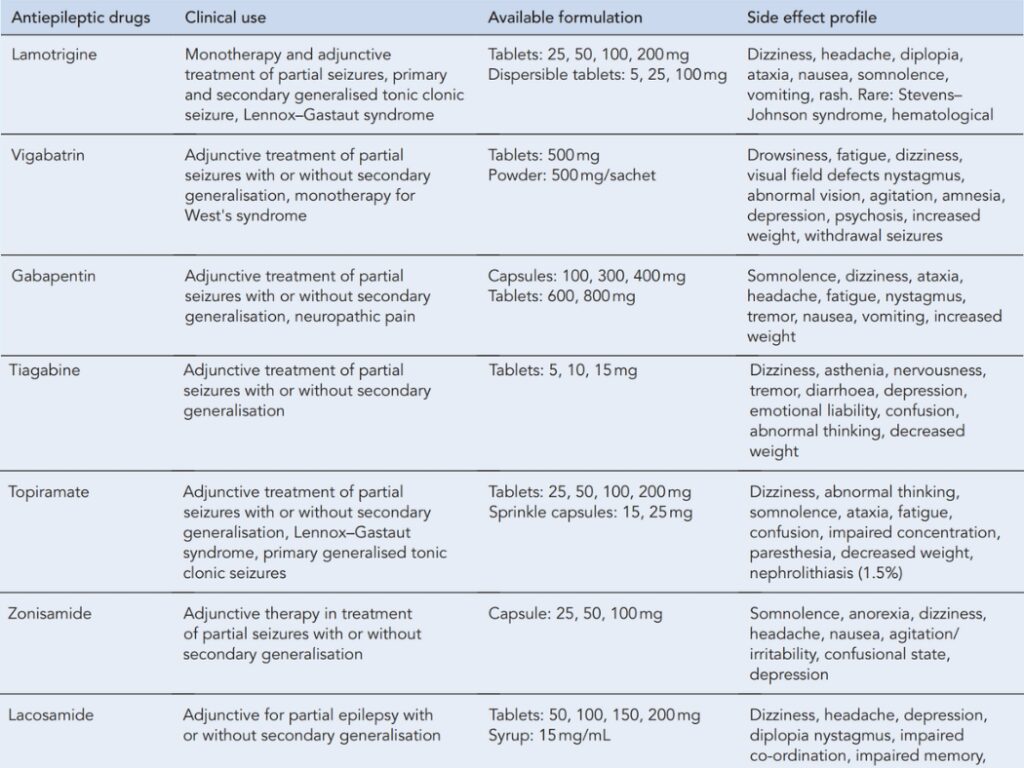
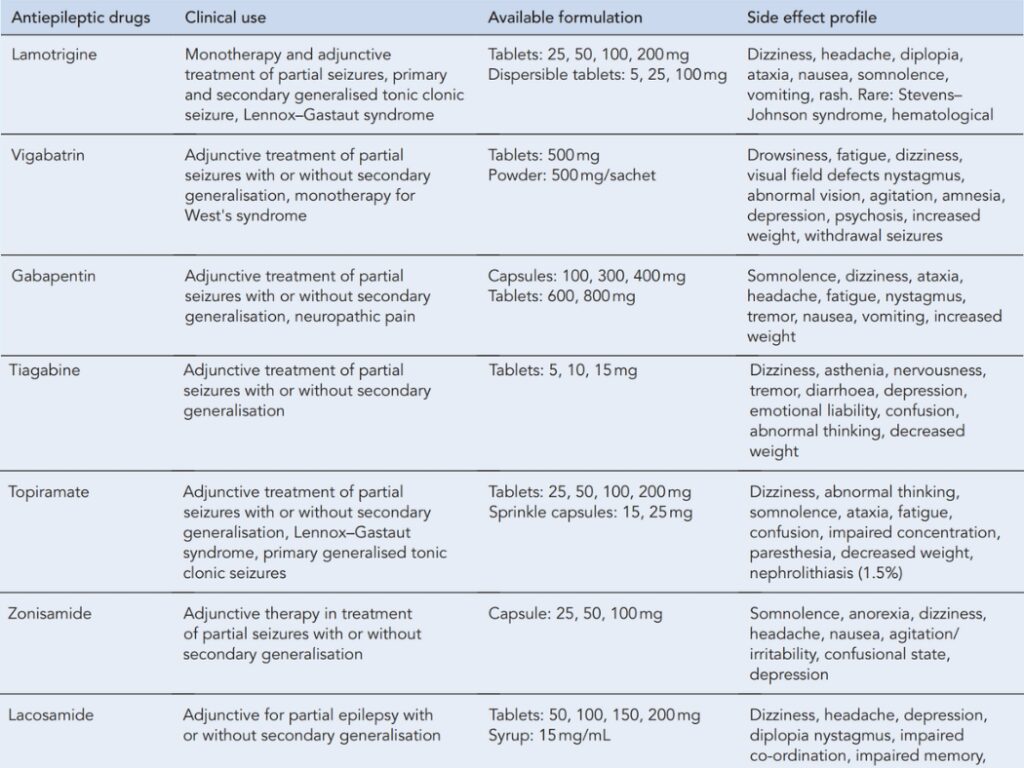
Initiation of therapy in newly diagnosed patients
The best first-line AED for the patient’s kind of seizure should be gradually started at a low dosage. This is because introducing anything too quickly could have unintended consequences that lose the trust of the individual. For the majority of medications, the patient should be convinced that a slow introduction will result in a therapeutic impact just as quickly as a quick one.
Maintenance dosage
No AED has a single ideal dosage that works for every patient. The necessary dosage differs depending on the individual and the medication. Medication should be started slowly and then gradually increased to the starting maintenance dosage.With phenytoin, however, greater caution is required because the relationship between serum level and dose is nonlinear and slight adjustments to dosage can have a significant impact on serum level.
Withdrawal of drugs
AEDs should not be abruptly discontinued. Rebound seizures can happen, especially with barbiturates and benzodiazepines. Individual AED withdrawals should be made gradually and step-by-step to prevent the onset of withdrawal symptoms (e.g. over a period of 2-3 months).Barbiturates like primidone and phenobarbital, as well as benzodiazepines like clobazam and clonazepam, carry an especially high risk. In situations where a drug needs to be stopped quickly, such as when there are potentially fatal adverse effects, diazepam or another benzodiazepine can be administered to help get through the withdrawal period.
Examples of withdrawal regimens are given below.
-
- Carbamazepine 100–200mg every 2 weeks (as part of a drug change) 100–200mg every 4 weeks (total withdrawal)
-
- Phenobarbital 15–30mg every 2 weeks (as part of a drug change) 15–30mg every 4 weeks (total withdrawal)
-
- Phenytoin 50mg every 2weeks (as part of a drug change) 50mg every 4weeks (total withdrawal)
-
- Sodium valproate 200–400mg every 2 weeks (as part of a drug change) 200–400mg every 4 weeks (total withdrawal)
-
- Ethosuximide 125–250mg every 2 weeks (as part of a drug change) 125–250mg every 4 weeks (total withdrawal)
The aforementioned regimens can be modified for usage in various contexts. People need to be constantly watched for any changes in the frequency of their seizures.
Key points on the diagnosis and management of epilepsy
A specialist with a focus on epilepsy should make an urgent diagnosis.
-
- EEG should be used to support the diagnosis.
-
- MRI should be used in adults who develop epilepsy, in whom focal onset is suspected, or in whom seizures persist.
-
- Seizure type(s), epilepsy syndrome, aetiology, and co-morbidity should be determined.
-
- A specialist should recommend appropriate treatment and start it as soon as possible. Treatment should be tailored to the individual’s preferences and lifestyle, as well as any specific needs.
-
- The individual with epilepsy, as well as their family and/or caregivers, should be involved in all decisions regarding their care, taking into account any special needs.
-
- Comprehensive care plans should be agreed upon.
-
- A structured review that occurs on a regular basis, at least once a year;
-
- A referral back to secondary or tertiary care for the patient in the event that:
-
- Epilepsy not well controlled;
-
- Pregnancy or contemplating pregnancy;
-
- Withdrawal of antiepileptic medication;
-
- A referral back to secondary or tertiary care for the patient in the event that:
-
- Magnetic resonance imaging (MRI);Electroencephalogram (EEG).