Diabetes Mellitus Type 2 (T2D), often referred to simply as Type 2 diabetes, is a prevalent and chronic medical condition that affects millions of individuals worldwide. Characterized by elevated blood sugar levels (hyperglycemia), T2D requires careful management to prevent complications and maintain a good quality of life. In this comprehensive guide, we will delve into the various aspects of T2D, including its causes, risk factors, symptoms, diagnosis, treatment, and prevention strategies.
Pathophysiology
A large percentage of people with type 2 diabetes have an accumulation of abdominal fat, which is physiologically distinct from subcutaneous fat and can result in “lipotoxicity.” The release of large amounts of free fatty acids from abdominal fat is resistant to the antilipolytic actions of insulin, which causes insulin resistance in the liver and muscle. The result is an increase in liver gluconeogenesis and a reduction in muscle insulin-mediated glucose absorption. Both of these lead to higher glucose levels in the blood.
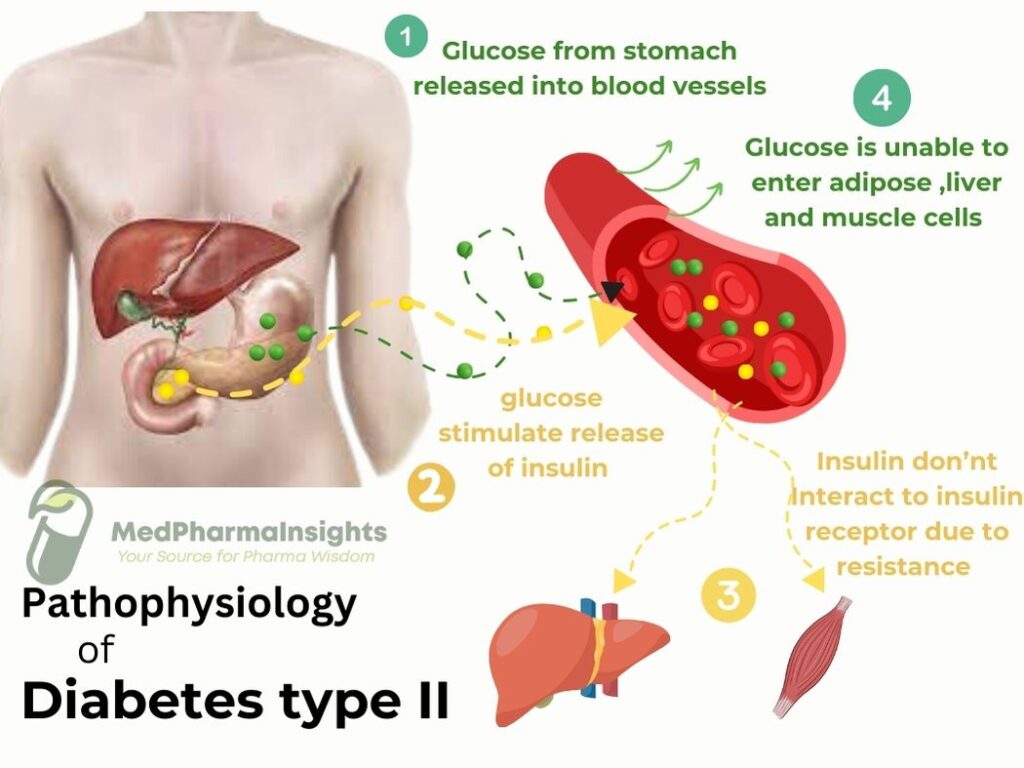
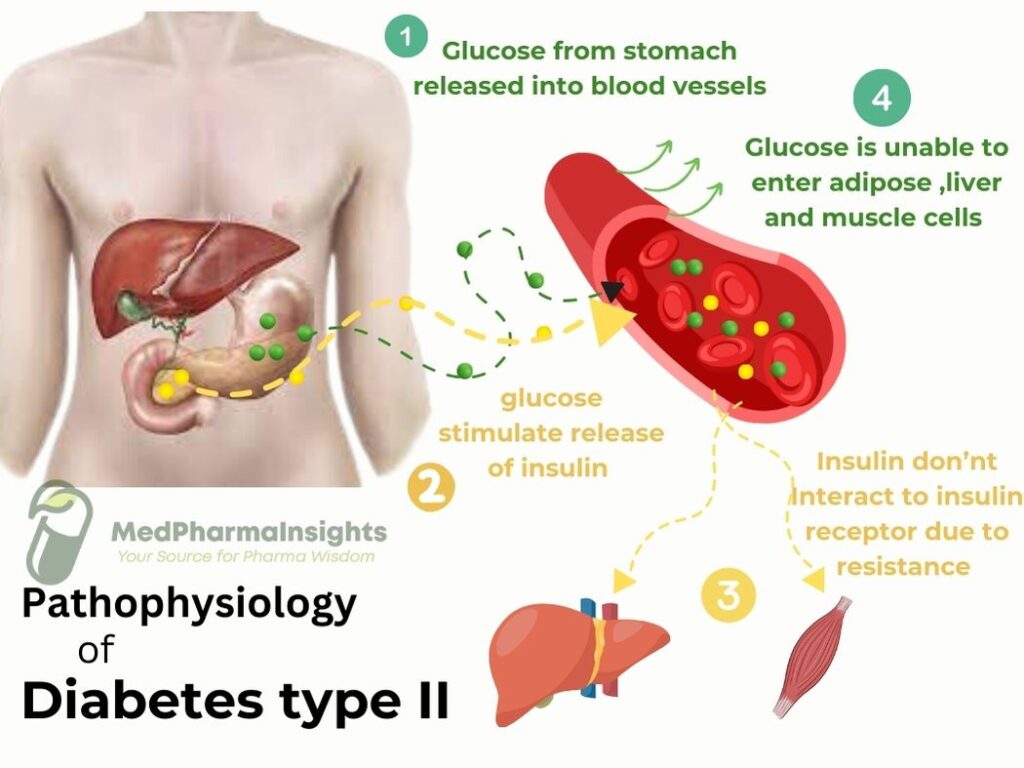
The accumulation of fat in the muscles, liver, and pancreas, which results in insulin resistance in these organs, is another way that excess fat itself may be a factor in insulin resistance. This is due to the fact that adipocytes grow into larger than normal, therefore they lose their ability to store any fat. Adipokines (also known as adipocytokines) known to cause inflammation, endothelial dysfunction, and thrombosis are oversecreted when there is too much intra-cavity adipose tissue. Example of Such adipokines include the prothrombotic plasminogen activator inhibitor-1 and the tumor necrosis factor and interleukin-6 (that are pro-inflammatory) ,resistin that brought Insulin resistance.
Hypercoagulability, poor fibrinolysis, endothelial damage (induced by persistent, subclinical inflammation), oxidative stress, and hyperglycemia all contribute to the atherosclerosis associated with insulin resistance. Additional adipose tissue is also believed to result in a essential adipokine’s undersecretion known as adiponectin. Adiponectin prevents monocytes from adhering to endothelial cells, preventing vascular injury. Adiponectin levels are lower in people with type 2 diabetes than they are in people without the disease, and weight loss raises adiponectin levels.
Causes and Risk Factors
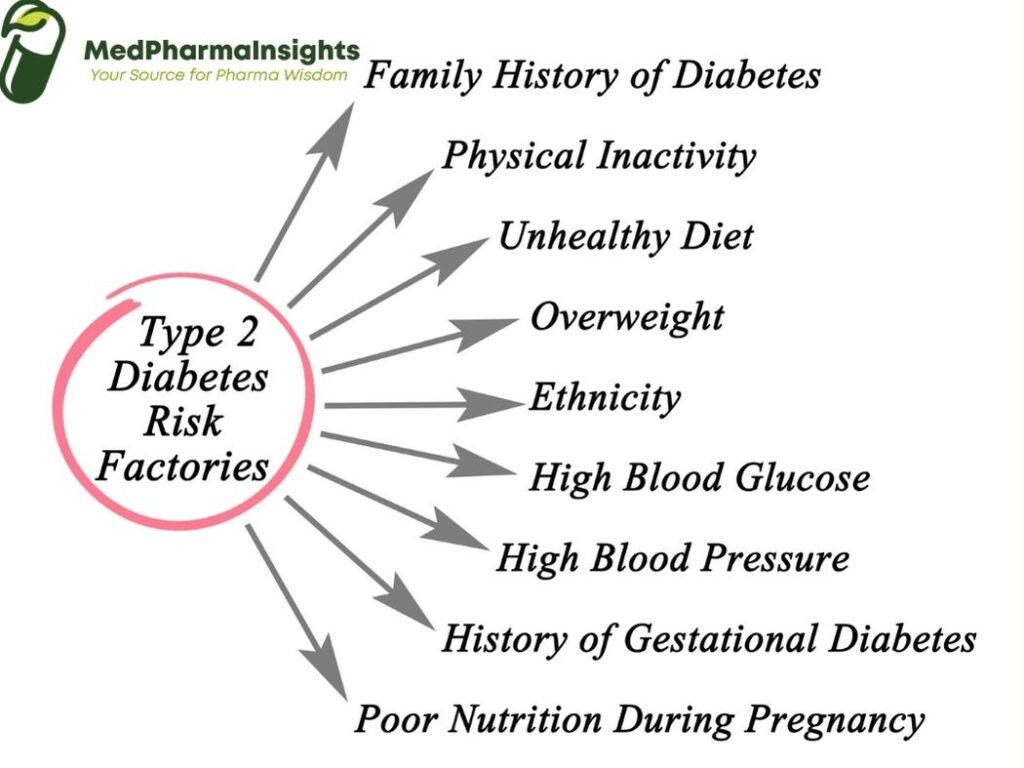
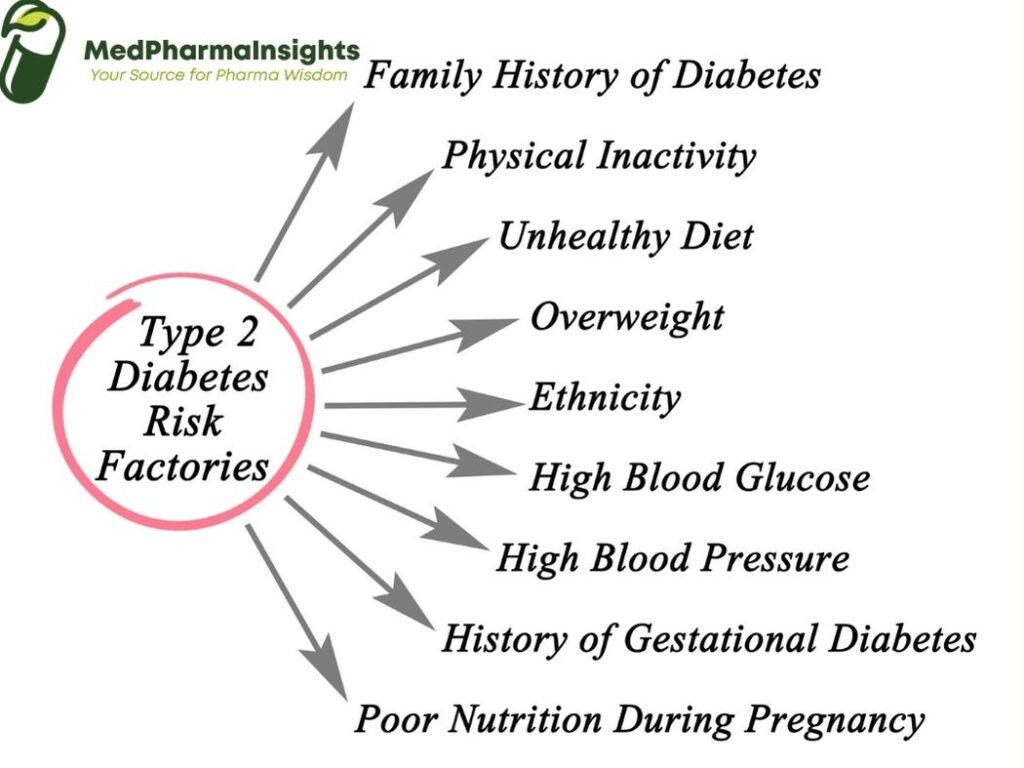
- Insulin Resistance: In T2D, cells become resistant to the action of insulin. This means that even though insulin is present, it is less effective in helping glucose enter cells.
- Genetics: Family history and genetic factors can increase the risk of developing T2D.
- Obesity: Excess body fat, particularly abdominal obesity, is a significant risk factor for T2D. Fat cells release chemicals that contribute to insulin resistance.
- Physical Inactivity: A sedentary lifestyle can lead to weight gain and insulin resistance.
- Poor Diet: Diets high in sugary and processed foods can contribute to insulin resistance and weight gain.
- Age: T2D is more common in people over 45, although it is increasingly diagnosed in younger individuals.
- Race/Ethnicity: Some racial and ethnic groups, such as African Americans, Hispanics, and Native Americans, have a higher risk of T2D.
Symptoms of T2D
- Frequent Urination (Polyuria): Individuals with T2D often experience an increased need to urinate, particularly at night. This is due to the kidneys attempting to eliminate excess glucose from the bloodstream through urine.
- Excessive Thirst (Polydipsia): The frequent urination associated with T2D can lead to dehydration, causing increased thirst as the body tries to compensate for fluid loss.
- Unexplained Weight Loss: Some individuals with T2D may experience unexplained weight loss, despite increased appetite. This can occur because the body’s cells are not efficiently using glucose for energy, leading to the breakdown of fat and muscle tissue.
- Increased Hunger (Polyphagia): Due to insulin resistance and inefficient glucose utilization, individuals with T2D may feel hungry more often, even shortly after eating.
- Fatigue: T2D can lead to feelings of fatigue and low energy levels, as the body’s cells are not receiving an adequate supply of glucose for energy production.
- Blurred Vision: Elevated blood sugar levels can cause changes in the shape of the eye’s lens, leading to temporary blurred vision.
- Slow Wound Healing: High blood sugar levels can impair the body’s ability to heal wounds and injuries, making the healing process slower than usual.
- Tingling or Numbness: Some individuals with T2D may experience tingling or numbness in their extremities, such as the hands and feet. This is often a sign of nerve damage (neuropathy) caused by prolonged exposure to high blood sugar levels.
- Recurrent Infections: T2D can weaken the immune system, making individuals more susceptible to infections, especially in the urinary tract, skin, and gums.
- Skin Changes: Skin conditions such as darkened patches (acanthosis nigricans), skin tags, and fungal infections may be more common in individuals with T2D.
Treatment and Management of Diabetes type II
A- Lifestyle Modifications: The Foundation of T2D Treatment
1-Dietary Changes:
- Balanced Diet: Opt for a well-balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Focus on fiber-rich foods to help control blood sugar levels.
- Carbohydrate Monitoring: Be mindful of carbohydrate intake, as carbohydrates have the most significant impact on blood sugar levels. Consider working with a registered dietitian to create a personalized meal plan.
- Portion Control: Pay attention to portion sizes to avoid overeating, which can lead to weight gain and blood sugar spikes.
- Meal Timing: Spread your meals throughout the day to help regulate blood sugar levels. Consider smaller, more frequent meals.
2- Regular Physical Activity
- Aerobic Exercise: Engage in regular aerobic exercises like walking, jogging, swimming, or cycling. Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
- Strength Training: Incorporate strength training exercises to build muscle mass, which can improve insulin sensitivity.
- Consistency: Consistency in physical activity is essential for long-term blood sugar control.
3- Weight Management
- Weight Loss: Achieving and maintaining a healthy weight is often a primary goal in T2D management. Even modest weight loss can have a significant impact on blood sugar control.
- Sustainable Approach: Focus on gradual, sustainable weight loss through a combination of diet and exercise. Crash diets are not recommended.
4- Monitoring Blood Sugar:
- Regular Testing: Keep track of your blood sugar levels as advised by your healthcare provider. Self-monitoring helps you understand how various factors affect your blood sugar.
- HbA1c Testing: This blood test provides an average of your blood sugar levels over several months, offering valuable information for treatment adjustments.
B- Medications for T2D Treatment
In some cases, lifestyle modifications alone may not be sufficient to control blood sugar levels, and medications may be prescribed. There are several categories of T2D medications, each with its unique mechanism of action:
Oral Medications:
- Metformin: Often the first-line treatment, Metformin helps reduce glucose production by the liver and improves insulin sensitivity.
- Sulfonylureas: These medications stimulate the pancreas to release more insulin.
- DPP-4 Inhibitors, SGLT-2 Inhibitors, and GLP-1 Receptor Agonists: These drugs work on various aspects of blood sugar regulation, such as reducing glucose reabsorption by the kidneys or increasing insulin release.
Injectable Medications
- Insulin: In some cases, insulin therapy may be necessary to supplement or replace natural insulin production.
Diagnosis
Several tests and criteria are used to diagnose T2D. These include:
Fasting Blood Sugar Test:
- Procedure: A blood sample is taken after an overnight fast.
- Diagnosis: T2D is typically diagnosed if fasting blood sugar levels are consistently at or above 126 milligrams per deciliter (mg/dL) on two separate occasions.
Oral Glucose Tolerance Test (OGTT
- Procedure: After an overnight fast, a blood sample is taken, and then a sugary drink is consumed. Blood sugar levels are tested at intervals over the next two hours.
- Diagnosis: T2D is diagnosed if blood sugar levels exceed 200 mg/dL two hours after drinking the glucose solution.
Hemoglobin A1c Test (HbA1c)
- Procedure: This blood test measures the average blood sugar levels over the past two to three months.
- Diagnosis: A diagnosis of T2D is typically made if the HbA1c level is 6.5% or higher.
Random Blood Sugar Test
- Procedure: A blood sample is taken at any time, regardless of fasting.
- Diagnosis: T2D may be diagnosed if random blood sugar levels are consistently above 200 mg/dL, accompanied by symptoms of diabetes.