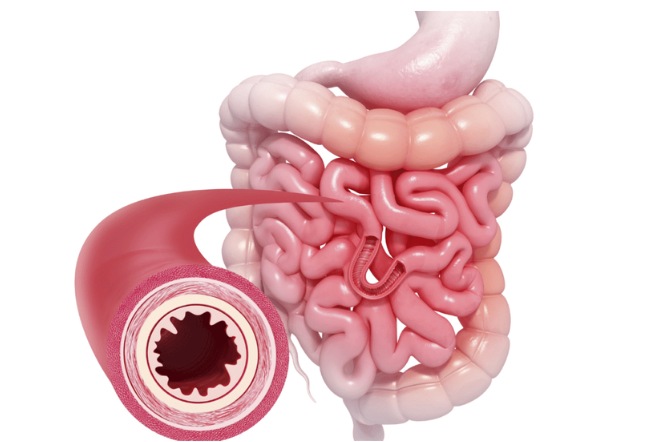
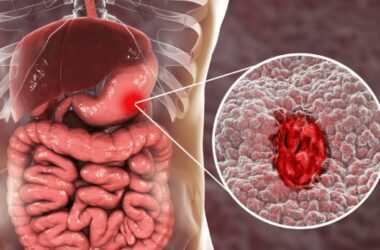
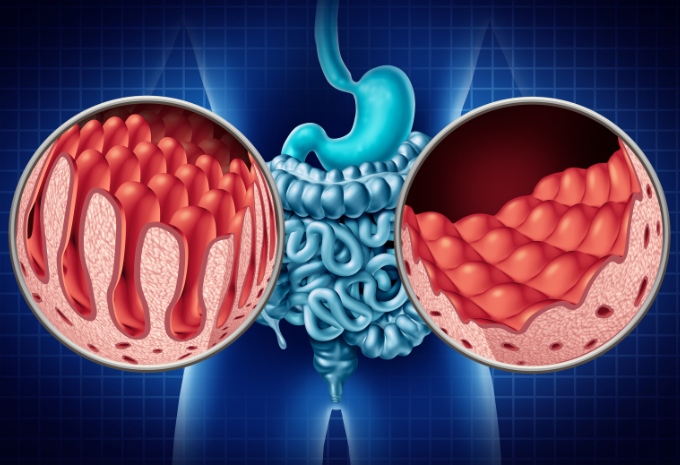
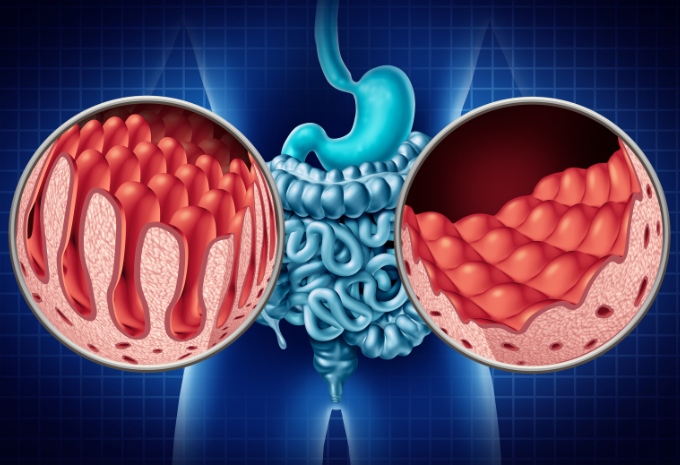
Inflammatory Bowel Disease (IBD) is a chronic medical illness characterized by inflammation of the gastrointestinal (GI) tract. It can be divided into two chronic inflammatory disorders of the gastrointestinal tract, namely Crohn’s disease (CD) and ulcerative colitis (UC). Crohn’s disease affects any part of the gastrointestinal tract, whereas ulcerative colitis only affects the colon and rectum.
The causative agents of IBD are largely unknown, although several factors are thought to play a role.
Environmental
Although many dietary factors, such as fat, fast food, milk, and fibre, as well as total protein and caloric intake, have been linked to IBD. Patients can identify which foods, such as milk or spicy meals, trigger or worsen their symptoms as their disease progresses. While patients with Crohn’s disease improve if they start taking elemental (amino acid-based), oligomeric (peptides), and polymeric (whole protein) feeds, symptoms may return when their regular diet is introduced. Up to 5% of ulcerative colitis patients improve by avoiding cow’s milk.
Smoking
Smoking has different effects on Crohn’s disease and ulcerative colitis, the two main forms of IBD. While smoking may increase the risk of Crohn’s disease, it appears to have a protective effect against ulcerative colitis. The risk of getting ulcerative colitis is most significant in those who used to smoke and lowest in people who currently smoke.
Enteric microflora
As a sensitizing organ that contributes to the systemic immune response, the gut plays a significant role in the development of IBD. This is because intestinal bacteria are present in the digestive tract. Since IBD patients lack immunological tolerance to intestinal microbiota, antibiotics frequently play a part in managing IBD. Probiotic, prebiotic, and symbiotic management of the intestinal flora has recently been found to be a successful therapeutic approach.
Drugs
NSAIDs like diclofenac, which are non-steroidal anti-inflammatory medicines, have been observed to worsen IBD. This is believed to be caused by direct suppression of the production of cytoprotective prostaglandins. Women who use the oral contraceptive pill are likely to have an increased risk of developing Crohn’s disease, which vascular abnormalities may bring on.
Stress
It has been demonstrated in animal models that stress might cause IBD to come back in some people. It is believed that stress causes enteric nerve endings in the gut wall to release inflammatory mediators.
Genetic
Since the middle of the 1990s, there has been a significant advancement in our knowledge of how genetics affect IBD phenotype and susceptibility. Small intestinal Crohn’s disease has been linked to mutations of the CARD15/NOD2 gene on chromosome 16 in white people but not in Asian ones. Recently, the genes DLG5 on chromosome 10 and OCTN1 on chromosome 5 were related to Crohn’s disease. IBD is more common among white people than black people in North America. A 10-fold increased risk of contracting the illness exists among first-degree relatives of people with IBD.
Hormonal Factors
Hormones may influence IBD, as the condition often occurs or worsens during periods of hormonal changes, such as puberty and pregnancy.
It’s important to note that IBD is a complex and multifactorial condition, and the interplay of these factors can vary among individuals. Additionally, there is ongoing research to better understand the precise mechanisms and causes of IBD. While the exact cause may not be known, effective management and treatment strategies are available to help individuals with IBD lead fulfilling lives and control their symptoms.