Celiac Disease is an autoimmune disorder that affects millions of people worldwide. It’s a condition that necessitates a strict and lifelong gluten-free diet. In this blog, we will explore the intricacies of Celiac Disease, from its causes and symptoms to its diagnosis and management.
Pathophysiology
The Role of Gluten
Celiac Disease is primarily triggered by the ingestion of gluten, a protein found in wheat, barley, rye, and their derivatives. Gluten is present in a wide range of foods, making it challenging for individuals with Celiac Disease to avoid.
Immune System Activation
The pathophysiology of Celiac Disease hinges on the body’s immune response to gluten. Here’s how it unfolds:
- Gluten Ingestion: When individuals with Celiac Disease consume gluten-containing foods, the gluten protein is broken down into smaller peptides during digestion.
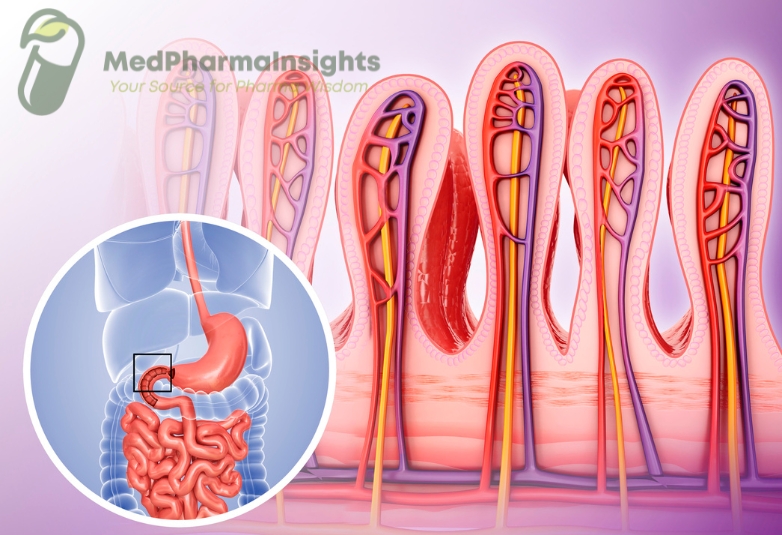
- Immune Recognition: Some of these gluten-derived peptides have structures similar to components of the body’s tissues, specifically a region of the small intestine called the lamina propria.
- Immune Activation: The immune system mistakes these gluten peptides for harmful invaders and mounts an immune response. This immune reaction primarily involves T cells and various antibodies, including anti-tissue transglutaminase (tTG) antibodies and anti-endomysial antibodies (EMA).
- Inflammatory Cascade: The immune response triggers an inflammatory cascade in the lining of the small intestine. This inflammation is characterized by the infiltration of immune cells and cytokine release.
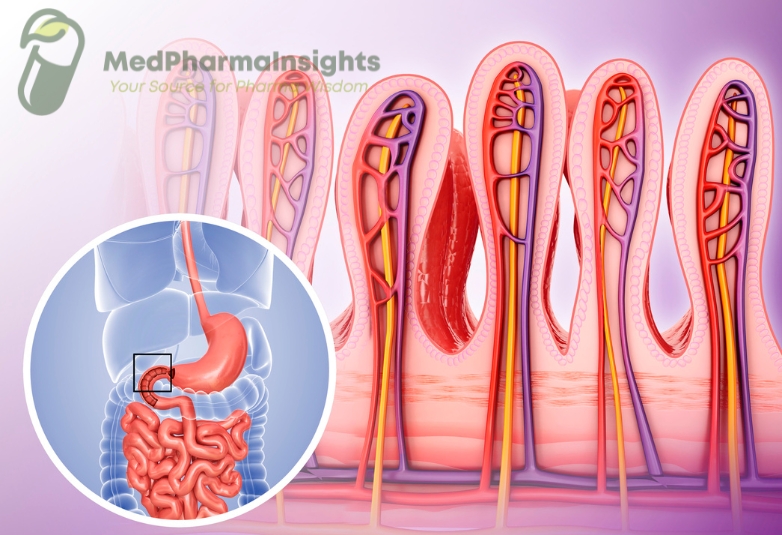
- Villous Atrophy: Prolonged and repeated immune activation leads to damage to the villi, which are finger-like projections lining the small intestine responsible for nutrient absorption. This damage is known as villous atrophy.
Impact on Nutrient Absorption
The damage to the small intestine’s villi disrupts the normal process of nutrient absorption. This can result in malabsorption of essential nutrients, leading to a range of symptoms, including:
- Chronic diarrhea
- Unexplained weight loss
- Anemia (due to iron or folate deficiency)
- Weakness and fatigue
- Muscle cramps
Causes and Risk Factors
The exact cause of Celiac Disease is not fully understood, but it is believed to involve a combination of genetic and environmental factors. Key points include:
- Genetics: Celiac Disease has a strong genetic component. It is more common in individuals who have a family history of the condition.
- Environmental Triggers: Gluten exposure is the primary environmental trigger. The disease may be triggered or exacerbated after viral infections, childbirth, surgery, or periods of severe stress.
Symptoms
Common Symptoms
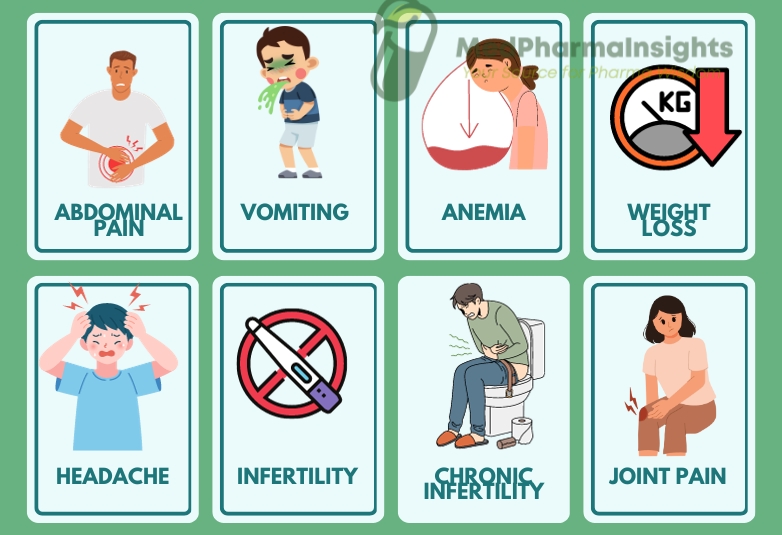
Celiac Disease can manifest with a wide range of symptoms, which can vary in severity among individuals. Common symptoms include:
Gastrointestinal Symptoms:
- Abdominal pain and bloating
- Chronic diarrhea
- Constipation
- Nausea and vomiting
Malabsorption Symptoms:
- Weight loss
- Fatigue
- Anemia (due to iron or folate deficiency)
- Weakness and muscle cramps
Non-Gastrointestinal Symptoms:
- Dermatitis herpetiformis (skin rash)
- Joint pain
- Headaches
- Osteoporosis or osteopenia
- Infertility or recurrent miscarriages
Diagnosis of Celiac Disease
1. Medical History and Physical Examination
Your healthcare provider will review your medical history and conduct a physical examination to assess your overall health and check for signs of nutritional deficiencies.
2. Blood Tests
- Blood tests are a critical step in diagnosing Celiac Disease. Specific antibodies, such as anti-tissue transglutaminase (tTG) antibodies and anti-endomysial antibodies (EMA), can indicate an immune reaction to gluten.
- Elevated levels of these antibodies in the blood suggest the need for further evaluation.
3. Small Intestinal Biopsy
- A small intestinal biopsy is considered the gold standard for confirming Celiac Disease. It involves an endoscopic procedure during which tiny tissue samples are collected from the lining of the small intestine.
- These tissue samples are then examined under a microscope for characteristic damage to the villi, which are finger-like projections that aid in nutrient absorption.
- Biopsy results that reveal villous atrophy or damage are a strong indicator of Celiac Disease.
4. Genetic Testing
Genetic testing can determine if you carry specific genetic markers associated with Celiac Disease, such as the HLA-DQ2 or HLA-DQ8 genes. However, genetic testing alone cannot diagnose the condition, as many individuals with these genes do not develop Celiac Disease.
5. Gluten Challenge
In some cases, if blood tests and biopsies are inconclusive, a gluten challenge may be recommended. This involves reintroducing gluten into the diet for a specific period, followed by retesting to assess the body’s response.
Treatment and Management of Celiac Disease
While a gluten-free diet remains non-negotiable, clinical pharmacology in Celiac Disease focuses on several aspects:
1. Symptomatic Relief
- Antacids and Proton Pump Inhibitors: These medications can alleviate acid reflux and heartburn symptoms, which are common in individuals with Celiac Disease.
- Anti-diarrheal Agents: For those experiencing chronic diarrhea, anti-diarrheal medications may provide temporary relief.
2. Nutritional Supplements
- Iron, Folate, and B-Vitamins: Many individuals with Celiac Disease experience nutrient deficiencies, such as iron and B-vitamin deficiencies. Supplements may be necessary to address these deficiencies.
- Calcium and Vitamin D: Osteoporosis is a potential complication of Celiac Disease. Supplements can help maintain bone health.
3. Immune Modulation
- Glucocorticoids (Corticosteroids): In rare cases of severe symptoms or complications, short-term use of glucocorticoids may help reduce inflammation and manage symptoms.
- Immunosuppressants: In cases of refractory Celiac Disease, where symptoms persist despite a strict gluten-free diet, immunosuppressive medications may be considered. These drugs aim to modulate the immune response.
4. Enzyme Therapy
Gluten-Digesting Enzymes: Researchers are exploring the development of enzymes that can help digest gluten more efficiently, potentially reducing the risk of accidental gluten exposure. However, these therapies are not yet widely available or approved for routine use.
5. Non-Dietary Adjunct Therapies
- Monoclonal Antibodies: Some research is focused on developing monoclonal antibodies that can target and neutralize gluten in the digestive tract, preventing immune system activation. These treatments are still in experimental stages.
- Vaccines: Investigational vaccines are being developed with the goal of inducing gluten tolerance in individuals with Celiac Disease. These are not yet available for routine clinical use.