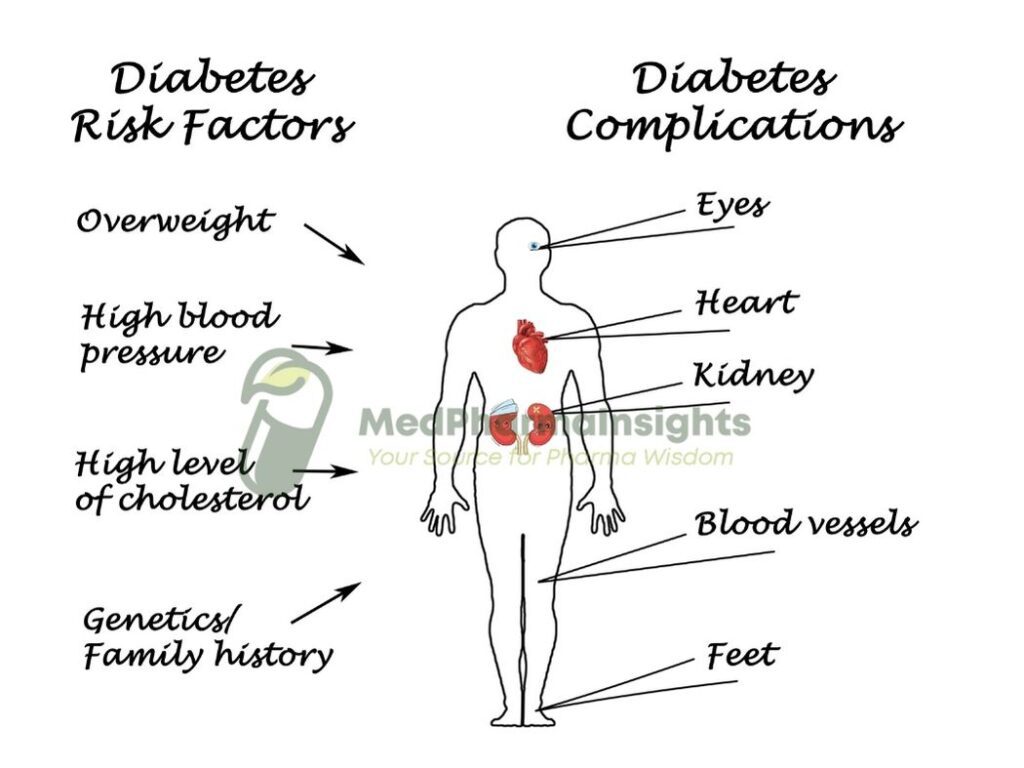
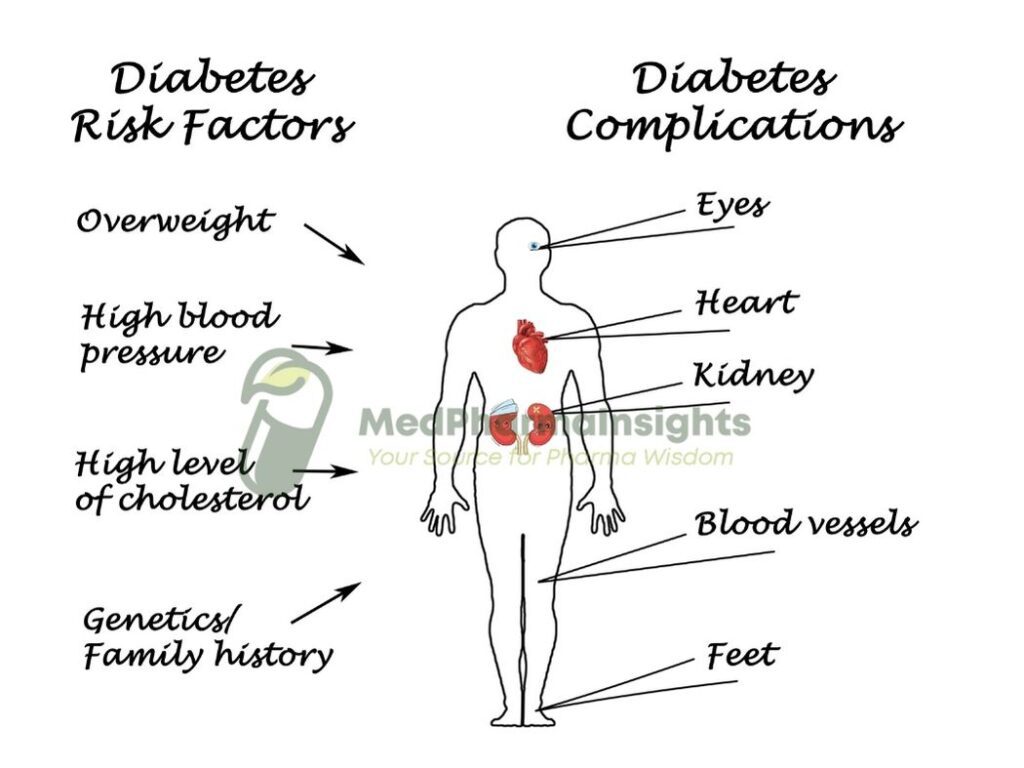
Diabetes is a chronic medical condition that affects millions of people worldwide. While the primary hallmark of diabetes is elevated blood sugar levels, this disease can wreak havoc on various organ systems in the body. Over time, uncontrolled diabetes can lead to a range of complications that impact a person’s overall health and quality of life. Although each kind of diabetes can lead to long-term problems, the range of incidence varies. Before receiving a diagnosis, many people with type 2 diabetes had already been afflicted for a considerable amount of time and had numerous diabetic problems. However, if proper management is implemented from an early stage, diabetic complications can be reduced and occasionally completely avoided.
Types of Diabetes
Before delving into the complications, it’s essential to understand that there are two main types of diabetes:
- Type 1 Diabetes (T1D): An autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. Individuals with T1D require insulin therapy for life.
- Type 2 Diabetes (T2D): Typically develops later in life and is characterized by insulin resistance, where the body’s cells don’t effectively use insulin. It may be managed with lifestyle changes, oral medications, or insulin.
Common Complications of Diabetes
Complications associated with diabetes can broadly be categorized into two types: acute and chronic. Acute complications can occur suddenly and have immediate consequences, while chronic complications develop over time due to long-term exposure to elevated blood sugar levels.
Acute Complications:
- Hypoglycemia (Low Blood Sugar): This occurs when blood sugar levels drop too low. It can lead to symptoms such as shakiness, confusion, sweating, and, if severe, loss of consciousness. Immediate treatment with glucose or sugar-containing foods is crucial.
- Hyperglycemia (High Blood Sugar): Elevated blood sugar levels can result in symptoms like increased thirst, frequent urination, fatigue, and blurred vision. Prolonged hyperglycemia can lead to diabetic ketoacidosis (DKA) in T1D and hyperosmolar hyperglycemic state (HHS) in T2D, both of which are medical emergencies
Chronic Complications:
There are two types of chronic diabetic complications: macrovascular and microvascular. Damage of large blood vessels results in macrovascular complications, while injuries to smaller blood vessels results in microvascular complications.
A- Macrovascular disease
The risk of macrovascular complications, including cardiovascular disease (coronary heart disease and stroke) and PVD, is 2–4 times higher for people with diabetes.
1- Cardiovascular disease
Cardiovascular disease is the leading cause mortality in patients with type 2 diabetes, accounting for an estimated 80% of fatalities in this patient population. The risk of having a myocardial infarction (MI) in person with diabetes is exactly the same as the possibility of getting a second MI in someone without diabetes. If nephropathy is present, the risk of cardiovascular disease is considerably elevated. Smokers are urged to give up, and people with hypertension and lipid problems are aggressively assessed and treated because these risk factors are exacerbated in the presence of diabetes. Diabetes increases the risk of silent myocardial infarction, which may be brought on by cardiac autonomic neuropathy.


2- Hypertension
In those with diabetes, hypertension is twofold as common as it is in the overall population. More than 80% of people with type 2 diabetes are impacted. People with diabetes typically have lower treatment goal ranges than those without diabetes because hypertension is linked to the emergence of macro- and microvascular problems. Hypertension is a component of the metabolic syndrome and is linked to insulin resistance in persons with type 2 diabetes. It is closely related to renal disease in those with type 1 illness.
3- Peripheral vascular disease
The blood arteries outside of the heart are affected by PVD. Diabetes frequently affects the arteries in the legs, which can result in intermittent claudication, or cramping when walking, which is caused by reversible muscle ischemia brought on by atherosclerosis. Erectile dysfunction and buttock pain can also result from iliac vascular damage. The risk of cardiovascular disease rises if PVD is present. Within two years of the onset of symptoms, myocardial infarction kills 20% of patients with PVD.PVD also causes a large portion of the morbidity linked to diabetic foot issues of the morbidity linked to diabetic foot issues is also caused by PVD.
B- Microvascular disease
1- Retinopathy
The kidneys expand and the glomerular filtration rate (GFR) initially rises in diabetic renal illness.The GFR begins to decrease as the nephropathy worsens, though. There are restrictions when using serum creatinine alone to gauge renal function. One can estimate the GFR (eGFR). The formula known as the Modification of Diet in Renal Disease (MDRD) is the most widely used and calls for the measurement of serum creatinine as well as information about age, sex, and ethnicity.
eGFR = glomerular filtration rate (mL / minper1.73m )
Microalbuminuria (the presence of minute amounts of albumin in the urine) is a sign of nephropathy. Proteinuria (also known as macroalbuminuria), which is indicated by larger levels of albumin, denotes more serious kidney impairment. An albumin:creatinine ratio (ACR) of 2.5 mg/mmol for men and 3.5 mg/mmol for women indicates microalbuminuria.An albumin:creatinine ratio higher than 30 mg/mmol or an albumin concentration higher than 200 mg/L can be used to define proteinuria.


Dialysis may be necessary if proteinuria leads to end-stage renal disease. Urinary albumin raises the risk of cardiovascular disease, with proteinuria posing a nine-fold risk, end-stage renal disease a fifty-fold risk, and microalbuminuria posing a two- to four-fold risk.
Nephropathy is less likely to develop when blood pressure and glycaemic levels are tightly controlled. The preferred treatments are ACE inhibitors and/or angiotensin receptor blockers (ARBs), both of which have been shown to have kidney protective benefits in addition to their antihypertensive effe
2- Nephropathy
The progressive loss of peripheral nerve fibers that causes nerve dysfunction is known as peripheral neuropathy. Numerous sensory, motor, and autonomic problems can be caused by diabetic neuropathies. The most typical variety is symmetrical distal sensory, which is most noticeable in the feet and may gradually lead to a total lack of feeling. Although it can occur with any type of diabetes and at any age after childhood, type 2 diabetes is the most common in elderly persons. Another form of sensory neuropathy is painful diabetic neuropathy, which can be very incapacitating and lead to significant morbidity.
Autonomic neuropathy may affect any part of the sympathetic or parasympathetic nervous systems. The most common manifestation is diabetic impotence. Bladder dysfunction usually manifests as loss of bladder tone with a large increase in volume. Diabetic diarrhoea is uncommon, but can be troublesome as it tends to occur at night. Gastroparesis may cause vomiting and delayed gastro-intestinal transit and variable food absorption, causing difficulty in the insulin-treated patient.
3- Peripheral neuropathy
Any component of the sympathetic or parasympathetic nervous systems may be impacted by autonomic neuropathy. The most typical symptom is impotence due to diabetes. Typically, bladder dysfunction presents as a decrease of bladder tone and a significant rise in volume. Despite being rare, diabetic diarrhea can be bothersome because it frequently happens at night. In a patient on insulin, gastroparesis can lead to vomiting, delayed gastrointestinal transit, and irregular meal absorption. Even though postural hypotension brought on by autonomic neuropathy is rare, it can be severe and incapacitating.
C- Macro- and microvascular disease combined
1- Diabetic foot problems
The majority of diabetes-related hospital bed-days are due to infected diabetic foot ulcers, which are also the most common non-trauma cause of amputations. Diabetes patients experience lower limb amputation at a rate that is 15 times greater than the overall population. A diabetic person has a 15% lifetime risk of having a foot ulcer. Diabetes-related foot ulcers are an expensive issue and have a high morbidity rate. Foot issues frequently occur from a confluence of distinct diabetes-related issues, including sensory and autonomic neuropathy, PVD, and hyperglycemia. Diabetes that is inadequately managed and poor foot care are additional contributing factors.
2- Charcot arthropathy
The majority of diabetes-related hospital bed-days are due to infected diabetic foot ulcers, which are also the most common non-trauma cause of amputations. Diabetes patients experience lower limb amputation at a rate that is 15 times greater than the overall population. A diabetic person has a 15% lifetime risk of having a foot ulcer. Diabetes-related foot ulcers are an expensive issue and have a high morbidity rate. Foot issues frequently occur from a confluence of distinct diabetes-related issues, including sensory and autonomic neuropathy, PVD, and hyperglycemia. Diabetes that is inadequately managed and poor foot care are additional contributing factors.